- Where does occur?
- What are the stages of endometriosis?
- Causes
- Risk factors
- How does it affect pregnancy and fertility?
- What is adenomyosis and how is it different from endometriosis?
- What conditions can it be related to?
- What can it be misdiagnosed as?
- Symptoms
- Diagnosis of Endometriosis
- Endometriosis Treatment
- Our approach to endometriosis
- Patient story
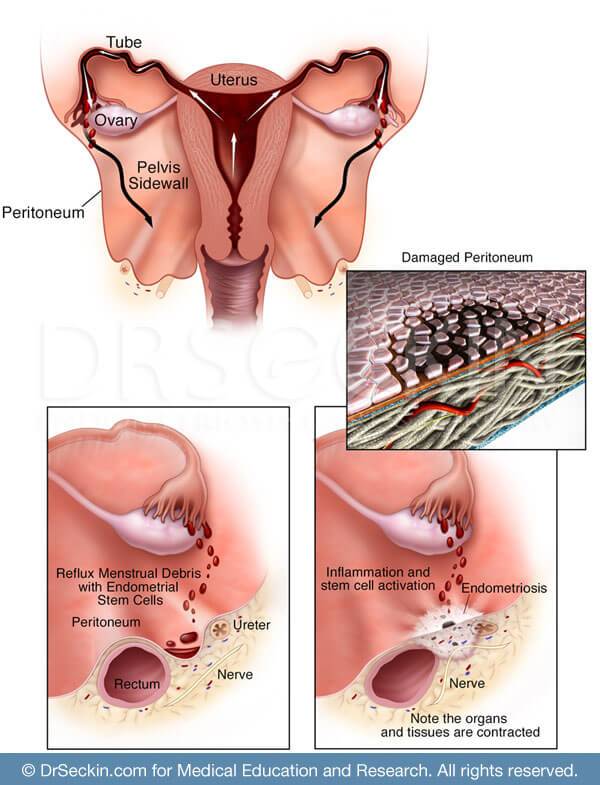
Endometriosis is a chronic disease in which endometrial-like tissue occurs outside of the uterus. This tissue, which normally lines the uterine cavity, is associated with monthly menstruation and is often characterized by abnormally painful and heavy periods, as well as pelvic pain, severe cramps, and pain with sex (dyspareunia). The lesions are estrogen-dependent, benign, inflammatory, stem-cell-driven, and at times progressive.
it affects an estimated 176 million women worldwide. A leading cause of infertility and chronic pelvic pain, it has also been linked to other health concerns, including certain autoimmune diseases and cancers, fibroids, adenomyosis, and interstitial cystitis. It is one of the leading reasons for laparoscopic surgery and hysterectomy in the United States. The economic impact of endometriosis is staggering. Businesses lose billions of dollars each year in compromised productivity and absenteeism because of the disease.
Where does occur?
it typically develops on the pelvic structures including the ovaries, fallopian tubes, bladder, and bowels (intestines).
It is also common for it to develop on the top of the vagina (anterior cul-de-sac) and in the peritoneal cavity between the rectum and the posterior wall of the uterus (posterior cul-de-sac).
In rare cases, it can spread to the diaphragm, lungs, kidney, appendix, and, surprisingly, the gastrocnemius (calf muscles).
What are the stages of endometriosis?
The American Society of Reproductive Medicine classifies endometriosis according to severity.
| Stages | American Society of Reproductive Medicine Severity Classifications |
|---|---|
| Stage I | Minimal |
| Stage II | Mild |
| Stage III | Moderate |
| Stage IV | Severe |
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Classifications
Because the four stages of endometriosis do not necessarily have any correlation to a patient’s symptoms or the nature of the infiltration itself, we often use a more descriptive system:
| Dr.Seckin’s Preferred Classification | Description |
|---|---|
| Early peritoneal |
|
| Ovarian endometriomas |
|
| Cul-de-sac obliteration |
|
| Deep infiltrating endometriosis (DIE) |
|
| Frozen pelvis |
|
Causes
The exact cause of endometriosis is not known. However, several plausible theories exist, including retrograde menstruation, Meyer’s theory, and more. We remain open to newly developing ideas.
Risk factors
While the following risk factors increase a woman’s risk of developing endometriosis, there are many cases in which women are diagnosed without any of the following:
- family history of the disease, especially in the mother or sister
- age (between 25 and 40)
- history of menstrual complications (i.e. long menstrual cycles, frequent periods)
- not having children
- high consumption of fats and red meat
- heavy alcohol intake
How does it affect pregnancy and fertility?
Endometriosis is likely responsible for one-third of infertility cases. The longer a woman has endometriosis, the more risk she has of infertility. However, up to 70% of women with mild to moderate endometriosis are still capable of conceiving
Adhesions on or near the ovaries, uterus, and fallopian tubes impede the transfer of the egg to the fallopian tube and may cause infertility. Moreover, ovarian implants may prevent the release of an egg and cause infertility. Finally, endometriosis can lead to a decrease in the number and quality of healthy eggs.
What is adenomyosis and how is it different from endometriosis?
Adenomyosis is endometriosis strictly within the uterine muscle. However, 50% of adenomyosis patients also have endometriosis
What conditions can it be related to?
Part of the reason why endometriosis is such a complex and dangerous condition is that it can lead to several other related conditions, including:
- adenomyosis
- adhesions
- ovarian cysts
- chronic pelvic pain
- infertility
What can it be misdiagnosed as?
Endometriosis can mask a number of conditions. It is often misdiagnosed and mistaken for the following conditions:
- IBS
- appendicitis
- hemorrhagic cysts
Symptoms
Endometriosis can cause the following symptoms.
- painful menstrual cramps (dysmenorrhea or “killer cramps”)
- heavy menstrual bleeding (menorrhagia)
- chronic pelvic pain
- pain with intercourse (dyspareunia)
- abdominal pain and bowel dysfunction including painful bowel movements, diarrhea, bloating, gas, or cramps
- bladder dysfunction, such as painful urination
- weakness, numbness, or pain in the nerves (neuropathy)
- fatigue
- infertility
- personality changes (depression, stress, apathy)
Diagnosis of Endometriosis
What is the first step towards diagnosing?
Before pursuing imaging, you should speak with a GYN physician who is familiar with diagnosing endometriosis and can provide a comprehensive pelvic exam. A physical exam and a discussion about your symptoms and medical history will help a physician determine if imaging tests are necessary.
What imaging tests are available?
In order to properly diagnose a patient with endometriosis and determine whether surgery is necessary, one or both of the following imaging tests must be conducted:
- ultrasound/sonogram
- MRI
What procedures and tests help definitively diagnose endometriosis?
In an operating room, a well-trained and experienced GYN surgeon will be able to visualize any anatomical abnormalities or endometriosis lesions through the following procedures:
While a physical exam and other imaging tests can give insight into whether or not a patient may have endometriosis, the only way to definitively diagnose endometriosis is through laparoscopic excision surgery. This must be accompanied by a biopsy sample that is sent to a pathology lab in order to confirm a diagnosis of the disease.
Endometriosis Treatment
There is currently no cure for endometriosis. However, there are surgical and non-surgical treatment options for pain and infertility caused by the disease.
Non-surgical methods to relieve symptoms
It is important to note that the following methods are not treatments for the disease, but rather may help control a patient’s pain and symptoms.
- painkillers
- acupuncture
- birth control pills
- anti-inflammatory diet
- medicated IUD
Surgical procedures
There are a variety of surgical treatments that a patient can undergo to treat endometriosis depending on the severity, stage, and quantity of the lesions.
| Technique | Description |
|---|---|
| Laparoscopic Deep Excision Surgery | The “gold standard” for removing all endometriosis in the body, ranging from lesions on the ovaries to the intestine |
| Myomectomy | Removal of fibroids, is necessary only when fibroids develop |
| Hysterectomy | Removal of the uterus, which is only needed in cases of diffuse endometrioma tissue in the uterus such as with adenomyosis |
Our approach to endometriosis
Endometriosis is not an easy condition to diagnose. Our practice provides a number of advantages.
- over 20 years of experience identifying, diagnosing, and treating endometriosis
- over 20 years of experience in laparoscopic deep excision surgery
- strong preference for laparoscopic deep excision surgery
- strong preference for excision surgery over robotics or laser ablation
- only performing hysterectomies or oophorectomy as the last resorts
- patented technologies, including the Aqua Blue Contrast technique (ABC)
- high-quality surgical imaging
Your health and well-being come first for us. With decades of experience, we know that this is the most important aspect of treating the disease and every patient is different and therefore every patient’s unique story and symptoms must be heard.
Patient story
Menoka M. has been experiencing severe pelvic pain for the past seven years and has not received a diagnosis for nearly five years. After seeing many doctors and having several surgeries, Menoka found us and was soon scheduled for laparoscopic deep excision surgery. Read about Menoka’s journey here, as well as how she is doing now.
You can read more stories of patients with endometriosis in our testimonial section.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.