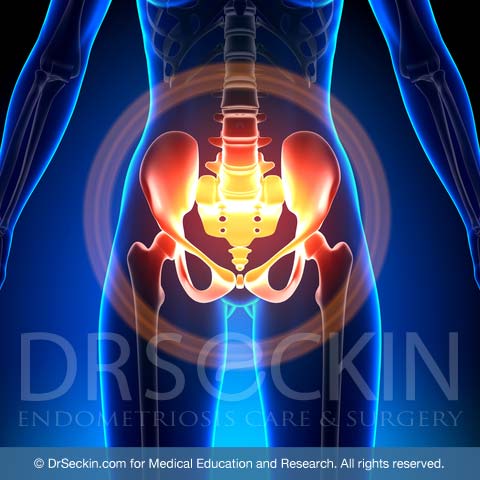
What is pelvic pain?
Pelvic pain originates from the nerves of tissues that make up the pelvis. These are bones, ligaments, muscles and organs are bladder, rectum , and uterus , tubes and ovaries. Pelvis is the lower part of the abdominal cavity, and all organs of the abdominal cavity, including pelvic organs is covered by peritoneum. All structures are supported with fine connective tissue with nerves and blood vessels. Fine nerve ending carry pain signals to the brain, then perceived as discomfort and pain. Normal functions if pelvic organs are not associated with pain. . Pelvic pain is a vital sign alerting a dysfunction of the single or multiple organs. Pelvic pain can also come with periods (dysmenorrhea), excessive menstrual bleeding (menorrhagia), and pain with sex (dyspareunia), all of which are common symptoms of endometriosis, along with bladder and rectal pain, painful bowel movements, constipation and diarrhea. Among others, sciatic and pudendal pain are certainly also signify deeper disease, and commonly associated with other components of pelvic pain.
Classification of pelvic pain
While there is no specific classification system for pelvic pain, there are different levels of pain and cramping that women may experience.
While most women experience mild cramps, not all cramps are painful. However, for women with endometriosis, symptoms will often be more excessive. This is because pain during menstruation can worsen with increased menstrual flow.
During the initial implantation stages of endometriosis, before deep infiltrating endometriosis or invasion, the pain is nonspecific and very commonly associated with gastrointestinal symptoms such as nausea, vomiting, bloating gas, or diarrhea.
In later stages of deep infiltrating and invading endometriosis, chronic pelvic pain can be accompanied by severe symptoms such as constipation, painful bowel movements, and painful intercourse. In fact, sometimes chronic pelvic pain can become so intense that it is referred to as “killer cramps”.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Causes of pelvic pain
A multitude of factors can cause female pelvic pain. However, it is very common that the cause is the dysfunction of abdominal and pelvic organs due to ovarian endometrioma or deeply infiltrating endometriosis.
Deeply infiltrating endometrioma leaves scar tissue on the abdominal and pelvic organs, as well as the peritoneum. This invading uterine tissue can ultimately play a role in organ dysfunction.

Endometriosis pain is always pelvic and usually occurs with menstruation.
Retrograde menstruation is the most common theory as to how endometriosis causes pelvic pain. Every month, the normal uterus sheds its lining (endometrium). The lining is then expelled out of the cervix with minimal backflow of the endometrial cavity contents. However, in some cases, the volume of menstrual debris that flows back up into the uterus is excessive and can lead to endometriomas growing in and scarring either the uterus and causing adenomyosis or areas outside of the uterus causing endometriosis.
There are many gynecological conditions that can cause pelvic pain. Nevertheless, researchers think that retrograde menstruation is also the main mechanism for these conditions.

Risk factors of pelvic pain
Having any of the following disorders, or a family history of them, can increase a patient’s chances of experiencing pelvic pain:
- endometriosis
- adenomyosis
- fibroids
Pelvic inflammatory disease (PID) is also a risk factor. PID is an infection of the female reproductive organs, such as the uterus, fallopian tubes, or ovaries. The main cause is sexually transmitted diseases that harm the vagina and spread internally to the uterus and other locations. It is one of the main preventable complications that can cause infertility.
The following are personal risk factors that can increase a patient’s risk of pelvic pain:
- physical or sexual abuse
- radiation or surgical treatment to the abdomen and/or pelvis
- anxiety, depression, or other psychosomatic symptoms
- miscarriages
- infertility
- long-lasting menstrual flow
Types of pelvic pain and associated complications
Women may experience pelvic pain in different forms. These could include cramps, especially during periods, dyspareunia, dysmenorrhea, painful bowel movements, and painful urination.
Pelvic pain can also cause complications such as vaginal and rectal bleeding, lower back pain, and infertility.
Diagnosing pelvic pain
Taking the patient’s medical history is the simplest way for a physician to gain an understanding of the severity and probable cause of pelvic pain. Provide as much information as possible about the type and frequency of the pain, and any other past medical or family history.
A pelvic exam can also help a doctor understand the intensity and point(s) of tenderness. This will be conducted in any comprehensive physical exam if a patient is displaying any gynecological signs or symptoms.
Your doctor will also most likely order lab tests along with conducting a comprehensive physical exam. These lab tests can include blood works, urinalysis, and other tests to check for any infection such as gonorrhea and chlamydia.
Imaging tests such as an ultrasound or sonogram that provides a picture of the inside of the uterus can also be useful in identifying endometriosis, adenomyosis, fibroids, and other intrauterine diseases that are impossible to detect via just pelvic exams and lab tests.
An MRI provides more clear and more precise imaging than ultrasound. It is extremely useful in confirming that a patient’s pelvic pain is likely due to diseases such as endometriosis or adenomyosis. However, due to its high cost, you should only have this test if your physician advises it following a comprehensive physical exam and lab tests.
Treatment of pelvic pain
It is crucial to first determine the cause of your pelvic pain, as it will determine your treatment plan.
Non-surgical treatments
There are a number of medications that can help relieve pelvic pain. These include painkillers, birth control pills, antibiotics, and antidepressants.
Painkillers may reduce pelvic pain in some cases. It is important to note that they will not treat the underlying cause of the pain. Painkillers range from analgesics such as nonsteroidal anti-inflammatory drugs like aspirin or ibuprofen to prescribed narcotics.
When a patient’s pain occurs during specific times in their menstrual cycle, birth control pills or hormonal medications may control it in some cases.
Doctors only prescribe antibiotics in case of pelvic pain due to infections.
Research has shown that antidepressants can reduce pelvic pain, even for patients who do not have depression. However, antidepressants primarily treat depression and do not address the pain itself.
Surgical treatment
When a patient’s pain is caused by endometriosis, adenomyosis, or fibroids as opposed to an infection, surgery is often the most advised method. The type of surgery can vary depending on the patient’s diagnosis.
Laparoscopic deep excision surgery, if performed well, is the best way to remove all scar tissue in cases of pelvic pain caused by endometriosis and focal adenomyosis.
Myomectomy removes fibroids, which in turn can relieve the pain.
Hysterectomy involves the partial or complete removal of the uterus. It is only necessary in cases of pelvic pain due to severe, diffuse adenomyosis. A hysterectomy should always be a last resort.
Our approach

Due to the myriad causes of pelvic pain, we believe that doctors must always first have a detailed discussion with their patients about their symptoms and medical history. This should be followed by a comprehensive pelvic exam and ultrasound. You are also advised to bring recent basic lab results and any imaging results, especially MRI. These will help us to better identify the probable cause of your pain.
When patients come to us, they are most often in need of surgical treatment. Our preferred method is laparoscopic deep excision surgery. Using this technique, we are able to remove all endometrioma and often able to relieve patients’ chronic pelvic pain. However, the pain can come from a variety of sources. It is important to find a surgeon who can not only operate with attention to detail, but also is patient and willing to discuss your medical history, symptoms, and complaints. By being open to discussion, we are able to work with our patients and find and treat the most probable source of their pain.
Patient story
Lindsay G. was experiencing severe pelvic pain for years. But she was told her symptoms were “just her.” After a history of ovarian cysts and surgical removal of one of her ovaries, Lindsay came to Dr. Seckin, who performed laparoscopic deep excision surgery on her in the spring of 2016. Read about Lindsay’s experience leading up to her surgery with Dr. Seckin.
You can read more patient stories in our testimonial section.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.