Ovarian endometriomas are highly common and may be present in up to 30-40% of women with endometriosis. Endometriomas are large, fluid-filled cysts that form on, and may even encapsulate, the ovaries.
How do ovarian endometriomas form?
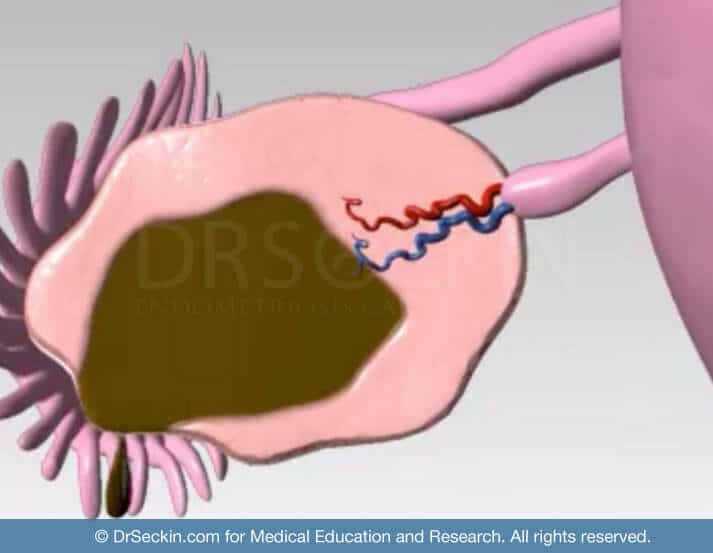
Retrograde menstruation is one of the possible causes of ovarian endometrioma formation. According to this theory, in cases of endometriosis, women have a higher rate of menstrual backflow. This causes blood to accumulate in the ovaries, ultimately leading to the formation of an endometrioma.
Why are ovarian endometriomas called “chocolate cysts?”
These sizable cystic masses consist of menstrual debris, including fragments of endometrial tissue, thickened blood, and inflammatory enzymes. These so-called “chocolate cysts”, aptly named for the appearance of the “old” blood they contain, may acutely rupture. This may cause their content to spill and adhere to the walls of nearby organs within the abdominal cavity.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Symptoms of ovarian endometrioma
All forms of endometriosis cause significant pain, infertility, and interruption of a woman’s ability to go about her normal daily routine. However, ovarian endometriomas can cause excruciating abdominal or pelvic pain.
Diagnosis of ovarian endometrioma
Some general practitioners may dismiss a patient’s symptoms and sonographic findings and attribute them to cysts. However, a proper diagnosis is very important as early intervention is the key to effectively resolving ovarian endometriomas.
Ovarian endometriomas also resemble hemorrhagic ovarian cysts. Moreover, due to the presence of a long asymptomatic stage, women usually receive a diagnosis late.
Treatment of ovarian endometrioma
Laparoscopic cystectomy can treat ovarian endometrioma. This involves the removal of the lining of the endometrioma cyst, ovarian reconstruction, and temporary ovarian suspension.
The ovarian cyst must be removed with precision without compromising the ovarian vascular supply.
The surgeon suspends the ovary for four to eight hours in the peritoneum following the operation so that it does not adhere to the pelvic sidewalls.
Despite these measures, ovarian function is usually lower after ovarian cystectomy due to the loss of ovarian follicles.
Is it possible to preserve ovarian function?
With proper adherence to meticulous techniques using microsurgical principles, we follow the strict guidelines of not using any electricity during ovarian surgery. We separate the cyst meticulously from the ovarian blood vessels. Using sutures rather than bipolar (electric) coagulation, we can reduce the loss of ovarian function.
Is it necessary to have my ovaries removed?
It is rarely ever necessary to remove the ovaries (oophorectomy) to remove ovarian or another form of endometrioma. An oophorectomy should be considered only if there is a suspicion of cancer, persistence of disease despite multiple previous cystectomies, and severe adhesions with deeply infiltrating pelvic sidewall disease-causing neuropathy.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.
