Our endometriosis specialists work with patients to understand symptoms, diagnosis, and treatment options for decide the best surgery techniques of endometriosis. This way we can use the best approach for endometriosis surgery for each individual patient.
Anatomical preservation and restoration
Endometriosis can alter the normal anatomy of organs through severe scarring, ultimately causing organ dysfunction. Scarring causes organs to fuse together, compromising their motility and autonomous functioning. Consequently, organ dysfunction allows endometriosis to infiltrate organs and organ systems even further.
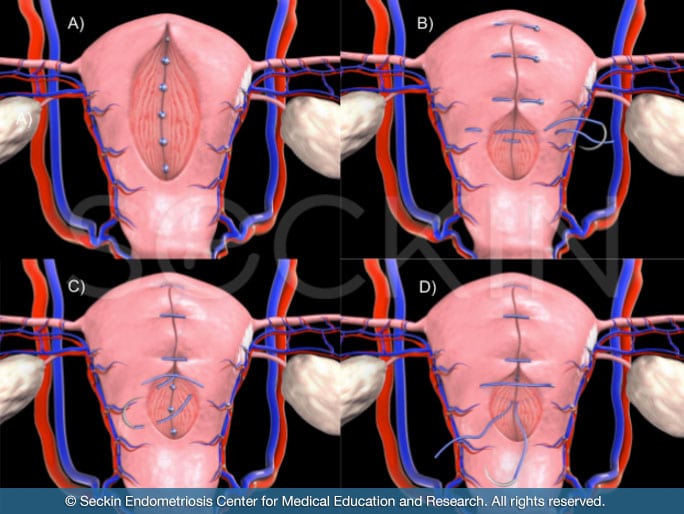
Using sophisticated visualization and imaging technology, Dr. Seckin examines individual lesions, excising endometriosis on a “per-lesion” basis. This allows for meticulous repair of the tissue, resulting in restoration of normal anatomical functioning. After excising lesions, he uses laparoscopic suturing to repair tissue and reconstruct organs.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Multiple organ excision
Endometriosis is classified as a multiple-organ disease. It can involve non-reproductive organs in addition to organs of the reproductive system, such as the bowels, bladder, diaphragm, kidneys, and, in rare cases, the lungs. This necessitates a multi-disciplinary surgical approach to address lesions that have spread beyond the reproductive organs. Bowel endometriosis, for example, is particularly complex and requires a multidisciplinary surgical team to provide comprehensive treatment. During this type of surgery, Dr. Seckin works with a team of highly skilled colorectal and urology specialists. This way, he minimizes the risk of postoperative complications and increases the likelihood of a successful outcome.
Conservative surgery
There are two surgical approaches to treating endometriosis: conservative and definitive surgery. Conservative surgery preserves organs such as the ovaries, ureters, and bowel. Despite the preservation of these organs, conservative surgery is not superficial surgery. It entails the thorough excision of endometriosis lesions without the need for organ removal. We perform conservative surgery for all patients with well-recognized endometriosis lesions, fibrotic lesions, and acute regions of inflammation.
In certain cases of deep infiltrating endometriosis and adenomyosis where nerve involvement and corresponding symptoms of neuropathy are likely, we resort to definitive surgical treatment. Definitive surgery involves organ removal. A hysterectomy, which is a definitive means of treatment for diffuse adenomyosis, is an example of definitive surgery. Removal of the ovaries (oophorectomy), bowels, part of the bladder, and reimplantation of the ureter, are all types of definitive endometriosis surgery.
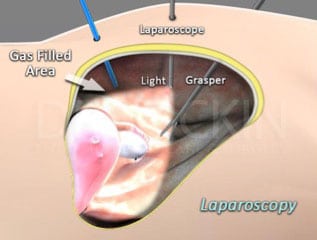
Laparoscopic deep excision surgery
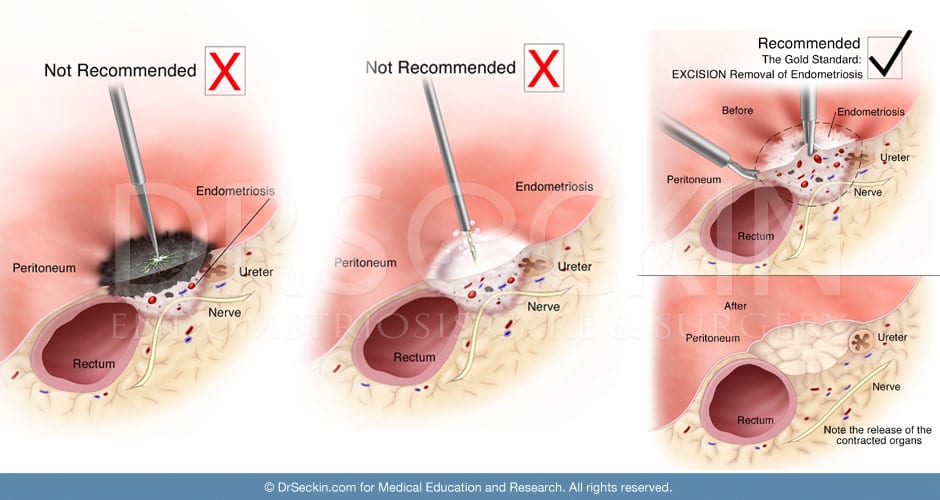
Known as “the gold standard” for endometriosis surgery, laparoscopic deep-excision surgery combines the standard surgical GYN imaging technique of laparoscopy with excision, a technique derived from the surgical removal of cancer (particularly breast cancer).
Excision surgery is our preferred method for removing endometriosis lesions. It is the only technique that removes the lesion in their entirety.
Methods of fulguration and laser ablation are only capable of removing lesions superficially. In other words, endometriosis tissue that lies beneath the surface of healthy tissue often stays behind. This increases the likelihood of symptom recurrence.
Deep excision surgery preserves the borders of healthy tissue surrounding the lesion. Methods of fulguration and laser ablation, on the other hand, present a risk of damaging surrounding tissue.
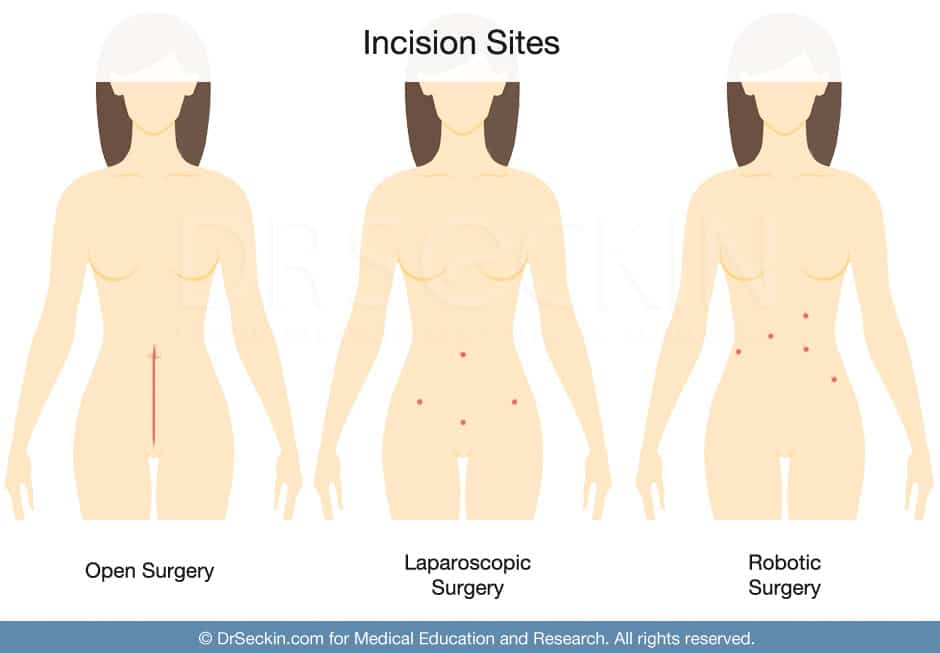
Minimally invasive surgery technique
We perform all our surgeries, even ones as complex as bowel endometriosis excision surgery, using the minimally invasive laparoscopic technique. This way, we aim to give our patients their best chance of symptom relief, recovery, and nearly-scarless results.
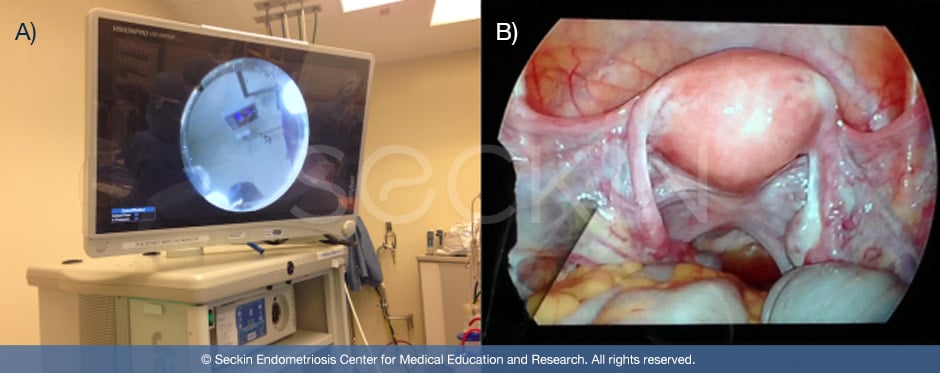
Aqua Blue Contrast (ABC) technique
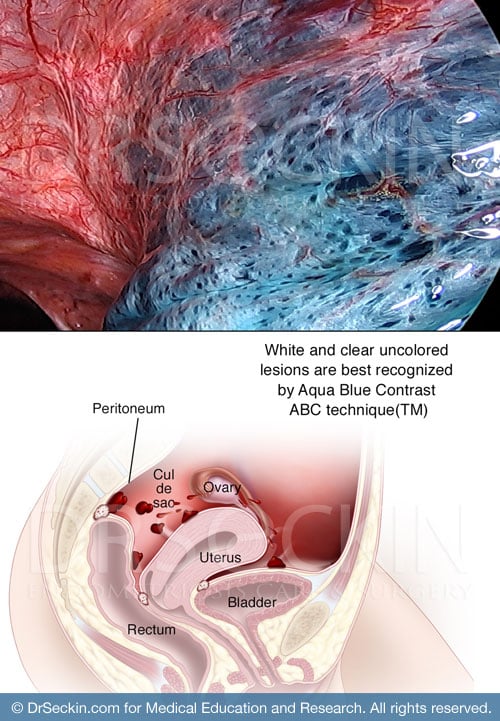
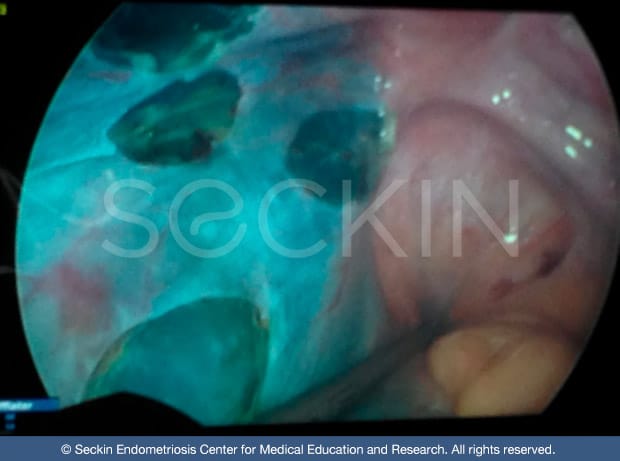
Another unique aspect of our excision surgery procedure is our use of Aqua Blue Contrast (ABC). We patented this technique specifically for endometriosis patients.
During surgery, we make a small incision into the peritoneum (lining of the abdominal cavity), a common site for endometriosis. We then fill this site with the ABC solution. The solution enhances the visibility of lesions that are difficult to see due to the intense brightness of the laparoscope light source.
We often compare our use of contrast to that of stars in the sky. During the day these stars are not visible, even though they are still present. However, when the sun’s light disappears at night, the stars become visible. Our contrast does the same to eliminate laparoscopic glare. This allows the surgeon to discern endometriosis lesions otherwise not visible to the naked eye. So they can identify and remove endometriosis that they would normally not be able to detect during normal laparoscopic surgery. As a result, patients see drastic results with symptom relief and have a lower chance of further endometriosis development.
“Cold” excision
Techniques of laser ablation and fulguration often rely on heat and electricity to destroy lesions. These often unnecessarily powerful energy sources can have damaging effects on surrounding healthy tissue and only remove lesions superficially. For these reasons, we exclusively use the “cold excision” technique. This technique excises the endometriosis lesions using minimal to no electricity and preserves the body’s healthy tissue.
With our method of cold excision surgery, we are also able to preserve removed lesions and send them to a pathology laboratory for testing at the cellular level for endometriosis. We feel this is a crucial component of our surgeries as it is the best way to definitively and formally diagnose endometriosis. It also helps us to better understand the possibility of lesions growing or spreading. With other surgical methods such as ablation, a pathology laboratory cannot test the endometriosis tissue because surgery often destroys it.
Robotic Surgery Techniques
Our surgeons are trained in the Da Vinci Surgical Systems and we perform surgery with both conventional laparoscopy or robotic technology.
We recognize that robotic surgery lacks certain haptic feedback and proprioception, but on the other hand, can offer an enhanced range of movement and increased surgeon comfort.
We are committed to the deep and meticulous excision of endometriosis. Certain procedures may benefit from one technique over the other and that would be discussed on a case-by-case basis during the surgical consultation. With all patients, we take care to minimize incisional scars for postoperative healing and cosmesis.
An integrated approach
Diet and lifestyle changes can constitute a complementary measure in the treatment of endometriosis, particularly for pre-and post-surgery patients. Because endometriosis causes widespread inflammation, which leads to symptoms such as constipation, diarrhea, abnormal gas, and bloating, patients may experience some symptom relief when following an anti-inflammatory diet.
In addition to dietary suggestions, we may complement surgical treatment with restorative pelvic floor therapy, osteopathic approaches for pain management, hormone therapy, and alternative therapies such as acupuncture and herbal medicine.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.