Hysterectomy is the surgical removal of the uterus. A total hysterectomy also includes the removal of the cervix. A supracervical hysterectomy preserves the cervix. Either way, it is a definitive surgical option and causes menstruation to cease.
With over three decades of experience in the field of gynecological surgery, the Seckin Endometriosis Center is one of the pioneers in laparoscopic hysterectomy surgery while ensuring minimal invasion.
We have been at the forefront of providing the proper technique for hysterectomies. We also constantly warn doctors and patients that the removal of the uterus should only be a last resort.
In the US, surgeons perform a hysterectomy in cases of multiple fibroids (40.7%), dysfunctional uterine bleeding (20%), uterine prolapse (14.5%), uncontrollable painful periods (10%), uterine cancer (9.2%), and endometrial hyperplasia (2.7%).
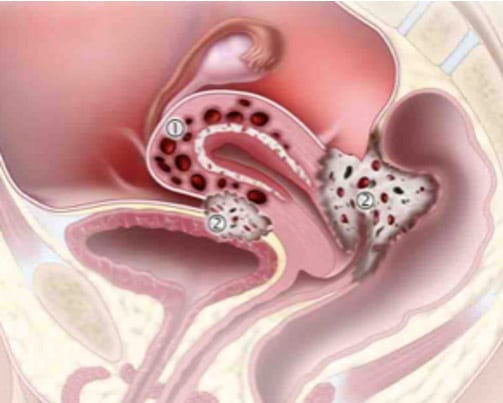
In the case of endometriosis, a hysterectomy is necessary if the disease heavily involves the uterus, a condition called diffuse adenomyosis. However, we often see patients who have had unnecessary hysterectomies, only to experience persistent symptoms as there are still lesions in the peritoneum, bowels, etc.
Hysterectomy should only be an option in patients who do not respond to conservative surgical therapy (such as excision of endometriosis implants) and do not want to preserve their fertility. In other words, a hysterectomy should be a last resort and only performed if absolutely necessary and unavoidable.
Regardless of whether a hysterectomy is necessary, it is imperative to also perform laparoscopic excision. This is to examine and remove all other adhesions outside of the uterus. Laparoscopic excision of endometriosis lesions outside the uterus is the gold standard treatment. It ensures patients the highest chance of symptom relief and recovery.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
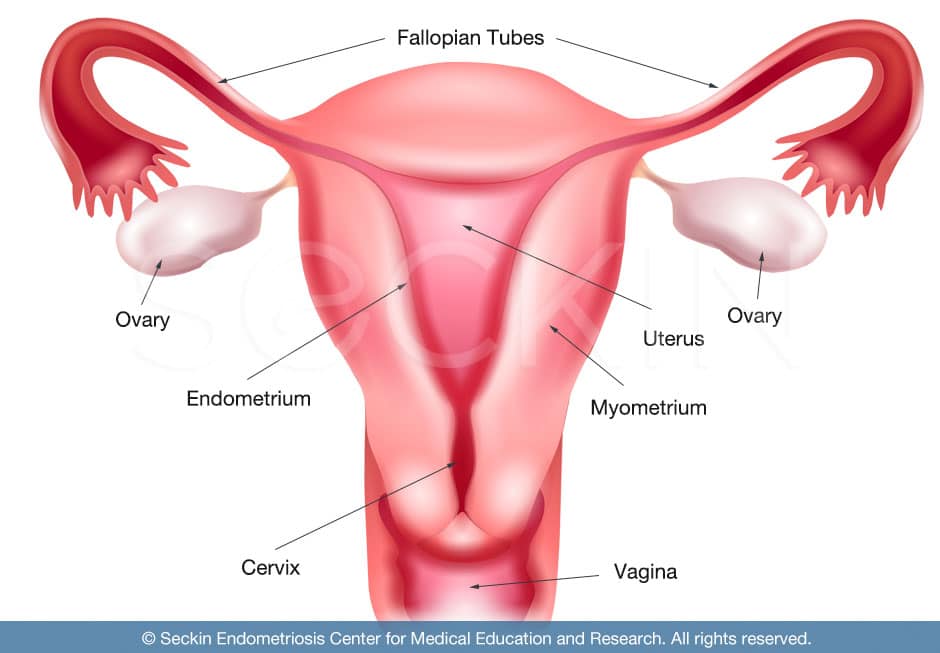
What is the function of the uterus and ovaries?
The uterus, the source of monthly menstruation, also houses a developing fetus. In the absence of pregnancy, a woman has about 400 menstrual cycles during her reproductive life. The ovaries are the sites of egg development Ovulation takes place, along with the production of estrogen and progesterone. Estrogen prepares the lining of the uterus for pregnancy in the first 14 days of the cycle. Progesterone then prepares the endometrium between days 14 to 28 of a cycle for the first step of pregnancy, implantation. When a sperm fertilizes an egg, the developing embryo travels down the fallopian tube and implants into the mature uterine lining. Then, the pregnancy continues to develop in the uterus for an average of nine months and ten days.
The uterus is not responsible for the production of estrogen, progesterone, or any other hormones. The ovaries produce these hormones and then feed them into the uterus.
Side effects of hysterectomy
The removal of the uterus eliminates the function it serves, which is to host pregnancy. Without the uterus, a woman will no longer have menstrual periods nor be able to bear children.
According to the Center for Disease Control and Prevention (CDC), the US has the highest rate of hysterectomy surgeries in the world, with more than 600,000 performed each year. In fact, approximately 300 out of every 100,000 women will undergo a hysterectomy at some point in their lives.
Why is a hysterectomy so common?
A hysterectomy rate of 0.3% may not seem high. However, it is the second most common surgery that women in the US undergo after a C-section. Some of the most experienced surgeons in the world argue that hysterectomies are amongst some of the most overperformed surgeries.
A great number of hysterectomies aim to ensure a patient will no longer suffer from disorders such as endometriosis. However, in most cases, a hysterectomy will not treat endometriosis. An endometriosis patient should always pursue laparoscopic excision surgery first, and should only consider a hysterectomy if absolutely necessary.
However, many doctors lack the experience, skill, and knowledge to perform laparoscopic excision surgery. Therefore, they settle on performing a hysterectomy. This is not a testament to how “good” or “bad” the doctor is, as they may not even be aware of this form of treatment. Nevertheless, this lack of knowledge is one of the primary reasons why hysterectomies are so common.
If you decide to have a hysterectomy, it is crucial to make sure you have exhausted all other surgical options and that there are no remaining endometriosis lesions in your body.
When is it necessary?
A hysterectomy should have justifiable indications. Pelvic pain may have multiple causes. In the absence of uterine disease, doctors and patients should be cautious in proceeding with a hysterectomy.
In addition, pre-operative tests like MRIs do have false sensitivity in detecting uterine pathologies such as endometriosis or adenomyosis. Therefore, any need for a hysterectomy should be confirmed with laparoscopic surgery. Nevertheless, there are several conditions where a hysterectomy is unavoidable. These are:
- multiple uterine fibroids
- recurrent fibroids after a myomectomy
- diffuse adenomyosis and extensive endometriosis
- cervical dysplasia (pre-inclination of cervical cancer)
- cervical cancer
- uterine cancer
What diagnostic tests can confirm these conditions?
| Diagnostic Test | Purpose |
|---|---|
| Endovaginal and abdominal sonogram | Intravaginal and abdominal ultrasound imaging will help confirm the presence and location of adenomyosis and fibroids, as well as help to determine the condition of the ovaries. |
| MRI and contrast | An MRI produces high-quality images of the body, which can give confirmation for a presumptive diagnosis of endometriosis, adenomyosis, and fibroids. This test allows your surgeon to visualize the status of the ureters, which serve as the kidney outlet to the bladder. |
| Dilation and curettage (D&C) | In the operating room, a surgeon will look inside your uterus with a video camera in order to rule out cervical or uterine cancer, diffuse adenomyosis, submucosal fibroids, or any other findings that call for a hysterectomy. |
Types of hysterectomy
The first laparoscopic hysterectomy was performed by Harry Reich in 1988. Since then, the technique has evolved to ensure minimal invasion. Hysterectomies can either be via the vagina or abdomen.
An abdominal hysterectomy (with a surgery route through the abdomen) requires varying lengths of visible incisional scarring.
A vaginal hysterectomy (with a surgery route through the vagina), causes almost no abdominal scarring. It is considered the best surgery route for a hysterectomy. However, not all uteruses can be removed via vaginal hysterectomy. This is because some may be too large, or the status of the ovaries and peritoneal disease may be unknown.
In laparoscopic hysterectomy, surgeons use a laparoscope to visualize the uterus, ovaries, and pelvic cavity via very small incisions they make through the abdomen. These incisions allow them to remove the uterus from the vagina. The laparoscopy gives a surgeon complete visualization of the pelvic anatomy. This allows him or her to remove any pathology outside the uterus involving the ovaries and fallopian tubes that they would not have seen if they performed a normal vaginal hysterectomy.
Proper pelvic floor suspension techniques are also performed during this time to lower the chance of prolapse. This technique is called laparoscopically assisted vaginal hysterectomy (LAVH).
What are the different classifications?
Aside from the route of the hysterectomy, there are specific techniques as to how to remove the uterus. While your doctor should always provide the best recommendation for your particular case, you should remember that you always have a choice. A hysterectomy is a very personal and emotionally-taxing surgery, and you should feel comfortable discussing your options. Here are a few options that your surgeon may suggest if a hysterectomy is a right procedure for you.
Supracervical hysterectomy (partial)
This procedure involves the removal of the uterus above the cervix. Surgeons refer to this as a “partial hysterectomy” as the cervix is preserved. Retention of the cervix usually improves patients’ outcomes in sexual function and pelvic support. Nevertheless, patients risk ongoing cyclic bleeding from the cervix or reoperation to remove the cervix in the future.
Hysterectomy (total)
This form of hysterectomy removes the uterus and the cervix but preserves the ovaries. Patients often think that ovary removal is standard in a hysterectomy procedure. But in reality, ovaries will only be removed if specified. Although the ovaries are preserved, surgical “menopause” will occur. This means that periods will cease. However, the ovaries will continue to produce key hormones such as progesterone and estrogen. As a result, menopause symptoms such as hot flashes, mood swings, and fatigue will not occur.
Hysterectomy with bilateral salpingo-oophorectomy
This procedure removes the uterus, fallopian tubes, and ovaries in their entirety. Only when the term salpingo-oophorectomy accompanies a hysterectomy are the fallopian tubes and ovaries also removed. With this procedure, the body goes through menopause. It no longer produces estrogen and progesterone and symptoms such as hot flashes, mood swings, and fatigue occur. This form of hysterectomy can have emotionally taxing consequences. It should, therefore, only be conducted if a patient chooses to have their ovaries removed.
Partial vs. total hysterectomy
A common misconception among patients concerns the difference between a partial and total hysterectomy. They may think that a partial hysterectomy involves the removal of the uterus while preserving the ovaries and that a total hysterectomy is the complete removal of the uterus, along with the ovaries. However, what patients refer to as a total hysterectomy is what surgeons call a total hysterectomy with bilateral salpingo-oophorectomy. In other words, the removal of the ovaries is not normally part of a hysterectomy procedure, unless specified.
When patients hear the term hysterectomy, they should not be concerned about losing their ovaries unless doctors mention bilateral salpingo-oophorectomy. When doctors use the term partial hysterectomy, they refer to the removal of the upper half of the uterus, while preserving the cervix. To surgeons, a total hysterectomy means the removal of the uterus in its entirety, which includes the cervix.
Will menopause occur following a hysterectomy?
One of the side effects of a hysterectomy is that a woman will no longer menstruate. This can bring on different symptoms depending on the form of hysterectomy.
In a partial or total hysterectomy, because the ovaries are preserved, estrogen and progesterone levels remain the same. In turn, “surgical menopause” takes place. A woman’s period stops due to the removal of the uterus. But menopause symptoms such as hot flashes, vaginal dryness, and mood swings do not occur as the ovaries remain. Female reproductive hormone levels are normal, and menopause symptoms do not surface.
This is not the case in hysterectomies with bilateral salpingo-oophorectomies, where the ovaries are not preserved. Removing the ovaries means the loss of estrogen and progesterone, thus normal hormonal menopause begins.
Strong consideration should be given to conserving the ovaries when possible. Therefore, it is imperative to carefully consider whether to seek an oophorectomy with your hysterectomy.
How will my hysterectomy type affect the day of surgery?
The hysterectomy technique that your surgeon performs can have consequential effects on the amount of scarring and how long your hospital stay and recovery time may be. Taking these factors into account, here is a list of hysterectomies from the most successful to the least successful.
- Laparoscopically assisted vaginal hysterectomy (LAVH): Maximum of three incisions that are 3-5 mm each, which guarantees no overnight stay at the hospital and a one-week recovery time. This also includes procedures such as a laparoscopic total hysterectomy (LTH) and laparoscopic supracervical hysterectomy (LSCH).
- Vaginal hysterectomy: Maximum of three incisions that are 10-12 cm each, which requires one overnight stay at the hospital and one to two weeks of recovery time.
- Robotic hysterectomy: Five incisions that are 8-12 mm each, which require one to two overnight stays at the hospital and two to four weeks of recovery time.
- Open abdominal hysterectomy: One large incision that is 10-12 inches, which requires three to five overnight stays at the hospital and six to eight weeks of recovery time.
Hysterectomy as a treatment for endometriosis
Is it necessary to treat endometriosis?
A hysterectomy is not always necessary to achieve a comprehensive treatment for endometriosis. This is a common misconception among many physicians and we cannot stress this enough.
First and foremost, the primary treatment of endometriosis should always be laparoscopic excision of all endometriotic lesions. Only in cases of endometriosis with diffuse adenomyosis, multiple fibroids with recurrence even after a myomectomy, and/or cervical or uterine cancer, is a hysterectomy necessary.
For a definitive treatment of endometriosis when hysterectomy is necessary, the surgeon should tailor the operation to relieve all symptoms and not just symptoms of suspected uterine origin. In other words, many surgeons misguidedly conduct hysterectomies to ensure the patient no longer suffers from further spreading of endometriotic tissue. However, the endometriotic lesions that have already spread throughout the body will go unremoved.
In cases of endometriosis requiring a hysterectomy, it is crucial that all extrauterine superficial and deep endometriosis is excised before a hysterectomy. This ensures that all possible causes of a patient’s symptoms are treated.
When is it necessary to treat endometriosis?
The surgical choice for the treatment of endometriosis with a hysterectomy depends on many factors. These include the patient’s age, the severity of her symptoms, and whether she wants to have children. These are all key factors in decision-making.
A thorough history and physical exam are necessary to determine these factors, as well as gauge the areas that the disease may affect in the pelvis.
Diagnostic testing, such as ultrasound imaging and MRI, are also useful tools in determining whether a hysterectomy is necessary. This is strictly in instances of diffuse adenomyosis with anterior and posterior cul-de-sac obliteration.
Nevertheless, a hysterectomy alone will not definitively cure endometriosis if other affected tissues in the pelvis are not also removed. Only in cases where women with endometriosis no longer wish to have children, and have already had conservative laparoscopic surgery, is a total hysterectomy with bilateral oophorectomy the definitive option. However, even in these cases, it is still crucial that excision surgery is performed for all visually recognized and suspected endometriosis tissues along with the hysterectomy. Depending on the expertise of the surgeon, ovarian conservation may also be an option.
FAQ
What can I expect on the day of surgery?
Once you and your physician have come to an agreement that a hysterectomy is a right choice for you, you must prepare for the day of surgery. Any trip to the operating room can be intimidating. So, we like to inform our patients about what to expect before coming in for their hysterectomy.
- Light bowel preparation is necessary the day before surgery. This entails taking a stool softener in the form of magnesium citrate in order to empty the bowels. When full, the bowels have a tendency of sticking to the uterus, especially in cases of extensive endometriosis such as stage 4 endometriosis and frozen pelvis. Light bowel preparation the night before surgery can make the bowels much more accessible for your surgeon.
- We also advise a predominantly liquid-based light dinner the night before surgery, with no oral intake after midnight.
- Expect to be in the hospital overnight or go home the same day.
- Near scarless surgery to the abdomen with three to four incisions, each less than ⅕ of an inch (5 mm). Our technique for post-surgery suturing models that of plastic surgery.
- We make no sutures requiring a follow-up appointment. Instead, we use “surgical band-aids” that can be removed two to three days following surgery.
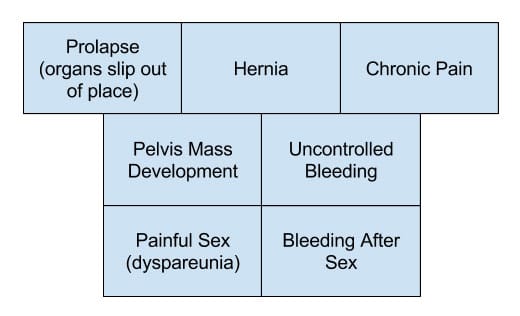
What are common complications that can arise late after the surgery?
What are key surgical aspects to avoid when choosing a hysterectomy surgeon?
Improper procedure
It is crucial to pick a hysterectomy procedure that suits your particular case. It is key to find a doctor who will have the patience and personability to have this type of discussion with you, while at the same time give you choices.
Avoid Robotics!
Never get sucked into the new and innovative treatments. Choose the best surgery: one that has the highest chance of success, while guaranteeing minimal invasion and high quality of care. In the case of cutting-edge technological treatments such as robotic surgery, there is a lower rate of success with larger incisions, and a higher number of incisions, than excision surgery performed in the hands of an experienced laparoscopic surgeon.
Many Large incisions
The best surgeons can perform a hysterectomy while ensuring minimal invasion. Having small and few incisions are always more preferred over large and many as it gives a lower chance of post-surgical scarring.
Inexperienced surgeon
Your surgeon should have great experience in hysterectomies. Any experienced surgeon will not only be able to perform the right hysterectomy procedure for you, but also make you feel comfortable while doing so.
Can I have sex after a hysterectomy?
It usually takes a maximum of six to eight weeks for a patient to heal following hysterectomy surgery, whether supracervical or total hysterectomy. Research has consistently shown that the majority of women have unchanged or improved sexual function one to two years after hysterectomy. Your surgeon should always go over proper postoperative care measurements to ensure you have a successful and time-efficient recovery period.
Our approach
How does our treatment ensure minimal invasion?
As one of the pioneers in the field of proper hysterectomy, and with over three decades of experience, we have mastered our technique to ensure minimal invasion. We found that the laparoscopic visualization required in proper uterus removal can be done without large or many incisions to the abdomen. Our technique ensures minimal invasion, in great part due to our world-renowned expertise in the field. We do not resort to invasive techniques such as robotic surgery. By not using robots, we are able to perform quicker, less risky, and overall more productive surgeries. Our results are nearly scarless.
Why do we prefer vaginal over abdominal hysterectomy?
Another component of our hysterectomy technique that makes our approach so unique is our expertise in performing laparoscopically assisted vaginal hysterectomies (LAVH). Most surgeons are not able to do this, especially when it comes to cases of endometriosis. This is because great skill and experience are necessary to do this successfully and without complications.
Before the uterus can be removed, a vaginal hysterectomy requires a surgeon to separately detach the uterus from the ovaries, fallopian tubes, upper vagina, as well as all the blood vessels and connective tissue that support it. Even in cases of endometriosis and diffuse adenomyosis, we perform all hysterectomies vaginally if possible. We do this by first excising all endometriosis lesions we can find throughout the pelvic and abdominal cavity. By performing laparoscopically assisted vaginal hysterectomies, we are able to see above the uterus anatomically. This gives us the ability to identify endometriosis lesions that we would not be able to see through a simple vaginal hysterectomy. Using this technique, we evaluate the peritoneum, cul-de-sac, and the uterus’s relationship with the ovaries and bowels.
The removal of the uterus through the vagina also ensures minimal invasion. When an abdominal hysterectomy is performed, a greater number of incisions that are larger in size must be made to remove the uterus through the abdomen. We have worked tirelessly to master the technique of vaginal hysterectomy so we can ensure minimal invasion.
How do we ensure that a patient’s symptoms disappear?
We firmly believe that whenever a hysterectomy is necessary in the case of endometriosis, thorough laparoscopic excision surgery should precede it. If a patient has endometriosis lesions, they should all be excised before the hysterectomy.
Many women come to us following hysterectomies with persistent symptoms. If a patient has endometriosis, simply removing the uterus does not address the many other regions where endometriosis may remain. In fact, the patient will most likely continue to experience symptoms as the disease spreads and pain worsens.
We take the time in the operating room to ensure that we excise all lesions and signs of endometriosis, even before we begin to remove the uterus. When we go into surgery, our primary goal is to not only remove the uterus but also ensure we are not doing so in vain. Our primary focus is always ensuring our patients have their highest chance of symptom relief. Laparoscopic deep excision of endometriosis is the best way to do so, with a hysterectomy only if absolutely necessary.
Why is a hysterectomy our last resort for treatment?
Once the uterus is taken out, it cannot be put back in, and a woman can no longer have children. This is why it can be such an emotionally difficult surgery to undergo and why we use it as an absolute last resort.
Unfortunately, many surgeons who are not familiar with endometriosis, especially those with no experience or even awareness of deep-excision surgery, do not have this mindset. They tell their patients that the only solution to their ailment is to remove the uterus. In many cases, this is either not true or not the full story.
While these may seem like small details to the average physician, to an experienced laparoscopic excision surgeon they mark the difference between a pointless hysterectomy and a highly successful excision surgery, with the possibility of preserving the uterus. This meticulous attention to detail makes a monumental difference in symptom relief following surgery. We make the decision only after thoroughly examining and removing all endometriosis lesions in the pelvic and abdominal cavity. To put it simply, we never perform pointless hysterectomies at Seckin Endometriosis Center.
We want our patients to have the highest chance of symptom relief and recovery, both physically and mentally. No patient wants to hear that a hysterectomy is the only option for them. We want to work with you to obtain a comprehensive and thorough understanding of your particular case to see if a hysterectomy is truly the right option for you. The first step towards this goal is through communication.
How this can help us choose the right method?
This same conservative approach also determines what specific type of hysterectomy we think is right for you. We always look to preserve the ovaries if possible. There is a potential higher risk of cardiovascular issues and bone loss in premenopausal patients with prophylactic bilateral salpingo-oophorectomy. As a result, hysterectomy and bilateral salpingo-oophorectomy is our last option. Nevertheless, this procedure can sometimes be necessary. However, even in those rare instances, we always have our patients’ approval, understanding, and consent. We always want our patients to know that they have a choice.
Patient story
Hysterectomy for advanced endometriosis (stage 4)
E.L was a patient in her early 40’s who quietly struggled with adenomyosis for nearly two years. After consulting with two other physicians, she underwent a successful supracervical hysterectomy treatment at Seckin Endometriosis Center. Learn about E.L’s story here.
You can read more stories of patients who received hysterectomies in our testimonial section.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.