Fibroids are benign (non-cancerous) tumors that grow on the muscle layers of the uterus. They can grow on the outside, inside, or within the smooth muscle of the uterine wall. A single fibroid is called a uterine fibroma. However, the term “fibroid” is more common as most cases involve six to seven fibromas on average. The fibroid mass primarily consists of smooth muscle and fibrous tissue, including extracellular matrix (i.e., collagen, fibronectin, and proteoglycan). Fibroids often cause an enlargement of the uterus itself, due to the fibromas stretching the walls of the uterus to be as large as that of a pregnant woman. A fibroma can vary in size from that of a small bean to as large as a melon. Other names incllude fibromyomas, fibromas, myofibromas, or myomas.
Classification of fibroids
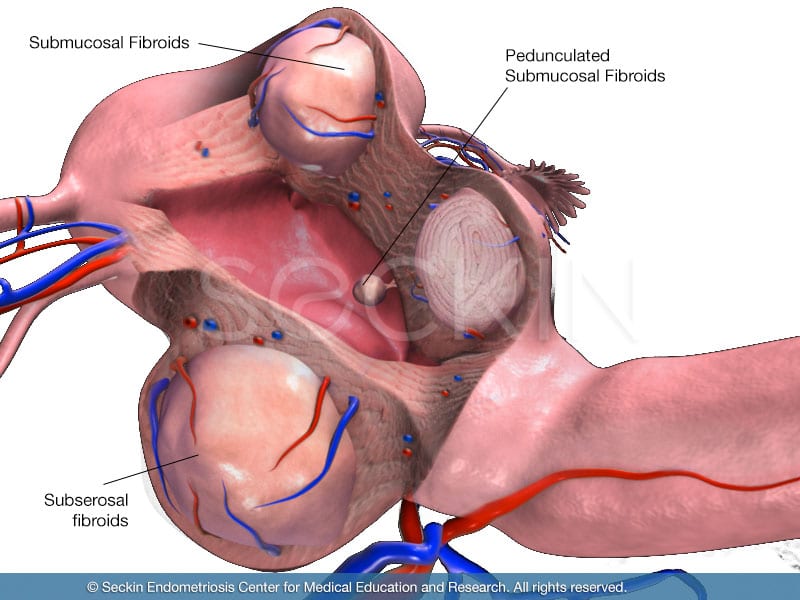
There are five different classifications: intramural, subserosal, submucosal, intracavity, and cervical.
Intramural fibroids
These are located in the thick wall of the uterus (myometrium) and are the most common type of fibroids, but also the easiest to remove.
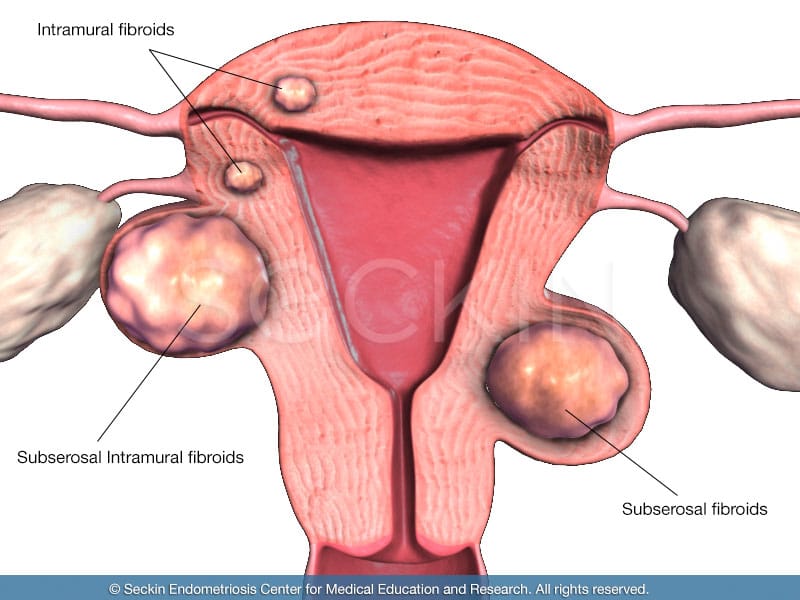
Subserosal fibroids
Located in the outer wall of the uterus, these can often grow to be the largest. They are one of two types of fibroids that can form a “stalk” on which the mass is attached (pedunculated fibroids).
Submucosal fibroids
These are located in the muscle beneath the lining of the uterine wall (endometrium). They also can form pedunculated fibroids.
Intracavity fibroids
These are located in the cavity of the uterus itself.
Cervical fibroids
These form in the cervix (the neck of the uterus).
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Causes of fibroids
There is no universal consensus on what precisely causes fibroids, but there are several theories.
Most recently, it has been observed that women who develop fibroids often have high estrogen and progesterone levels, which occur primarily during pregnancy. Moreover, when estrogen levels are low such as during menopause, fibroids tend to shrink. When estrogen levels are high, they swell. This theory is the prime reasoning as to why it is common to see overweight women develop fibroids.
A higher state of body fat means there is an excess conversion of the body’s sex steroids to the estrogen equivalent, estrone. IHigh levels of estrogen and estrone may play a key role in fibroid development and growth. The production of estrone is common in overweight women because fat cells contain the key enzyme aromatase, which is responsible for this conversion. Other growth factors, such as insulin-like growth factor (IGF) may also play a role in fibroid development. Meanwhile, many researchers think that there is a significant genetic component to fibroids because they can often occur in women with a family history of the disease.
Risk factors
Fibroids affect at least 20% of women (one in five) at some point in their lives. They develop in one in 100 premenopausal women, versus one in 1,000 women after menopause.
They are nine times more likely to develop in women of Afro-Caribbean descent (although racial differences in socioeconomic status and access to healthcare are a probable contribution to this discrepancy).
Women between ages, 30 and 50 are more likely to develop fibroids. Being obese or overweight can also increase a woman’s risk of developing fibroids. Finally, genetics/heredity may play a role.
Fibroids and pregnancy
For the most part, fibroids do not usually affect pregnancy. Nevertheless, there are some instances in which they can make conception difficult and even lead to miscarriages. When they physically distort the uterine cavity, several complications can arise, including infertility, recurrent miscarriages, premature labor, or complications of labor. As a result, in the case of large symptomatic fibroids, women may often choose to undergo an imaging review of the uterus via hysteroscopy or hysterosalpingography.
Fibroids may also press against and block the entrance to the fallopian tubes, subsequently preventing the egg from reaching the uterus. When they block the birth canal, they can interfere with labor and delivery, causing the need for a Caesarean section. Finally, they can prolong post-delivery recovery as they can increase heavy bleeding and the time it takes for a woman’s womb to return to its normal shape and size.
It is also important to note that pregnancy can cause fibroids to develop due to the elevated levels of progesterone and estrogen. However, there is little evidence to support this theory. Pregnancy may also cause “red degeneration.” This condition cuts off the fibroids’ blood supply and causes the fibromas to turn red and die, subsequently triggering intense abdominal pain and contractions of the womb that can lead to miscarriages.

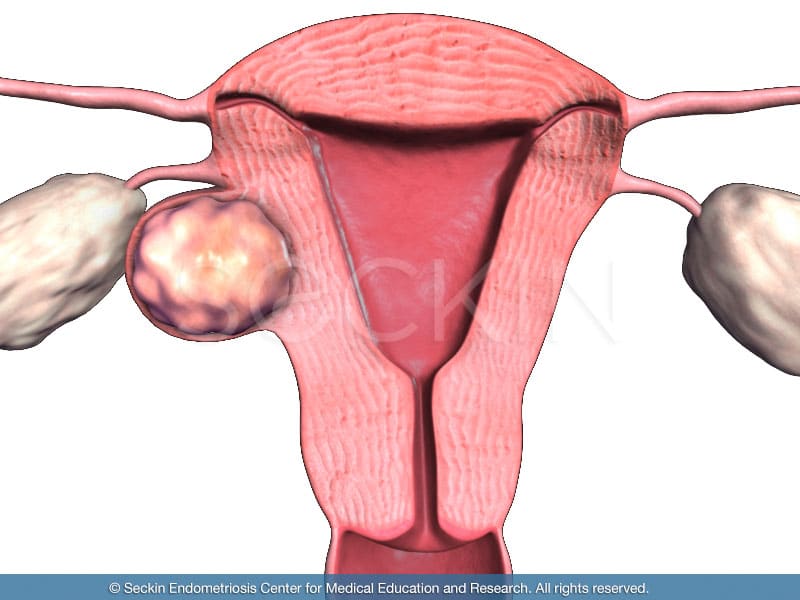
The “reddening” fibromas can be easily seen here using Dr. Seckin’s patented aqua blue contrast.
Congruent disorders
Benign fibromas (leiomyomas) can transform into leiomyosarcomas, malignant smooth muscle tumors in the uterus, in about 0.1% of cases. A pathological exam is the only way to observe this rare transformation. Patients with fibroids often present with anemia.
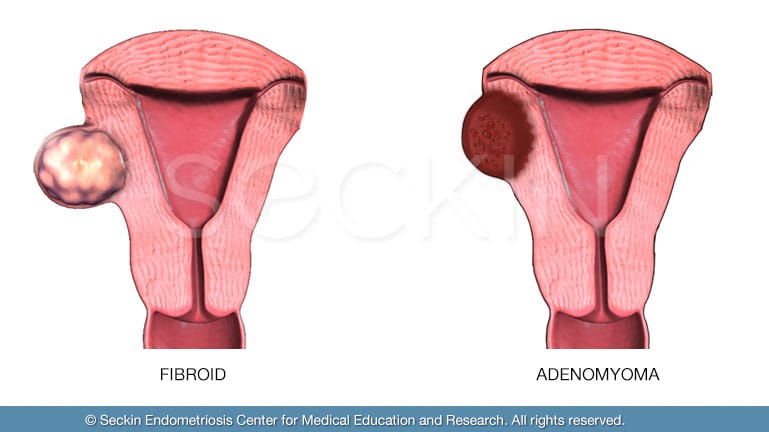
Fibroids vs. Adenomyosis
There are many cases in which doctors misdiagnose fibroids as adenomyosis or vice versa. However, fibroids are more of a focal condition in which benign singular fibromas arise in several areas of the uterus. Adenomyosis, on the other hand, is usually more diffuse. Even in cases of focal adenomyosis and adenomyoma adenomyosis, the diseased areas are more spread out and contain small pools of blood as opposed to the single, focal mass that is a fibroma. Adenomyosis is ultimately much more challenging and “messier” to remove with excision surgery.
Symptoms of fibroids
- heavy and prolonged menstrual bleeding (menorrhagia), which can include clots.
- a feeling of pressure in the pelvis, which can cause abdominal pain, back pain, and bladder and/or bowel dysfunction such as frequent urination, urinary urgency, urinary incontinence or leakage, difficulty emptying the bladder, constipation, hemorrhoids
- abdominal bloating
- infertility
- anemia
- fatigue
- dyspareunia
- deep thigh aches with varicose veins
In 75% of women diagnosed with fibroids, there are no symptoms at all.
Differences in symptoms may be due to the varying size and location of the fibromas.
Diagnosis of fibroids
Fibroids can be visualized indirectly or directly
Indirect visualization
Like in the case of adenomyosis, an ultrasound (sonogram) is the imaging technique most commonly used to diagnose fibroids. While adenomyosis often appears as diffuse thickening of the uterine wall, fibroids appear as round areas with a discrete border. There are two forms of ultrasound used to diagnose adenomyosis. These are abdominal and vaginal ultrasounds. An abdominal pelvic ultrasound can help find large fibroids. A transvaginal ultrasound is a bit more invasive but can detect small, more nuanced ones.
While ultrasound may be the most common technique, magnetic resonance imaging (MRI) is the most powerful. MRI can distinguish leiomyomas from other intramural lesions. However, in the case of endometriosis, most physicians choose to conduct an ultrasound before an MRI because it can be done in an office setting and is far less expensive.
Direct visualization
Direct visualization techniques are more invasive and expensive than an ultrasound or MRI. They are usually performed along with surgeries or in case of highly concerning symptoms. Nevertheless, they provide clear and direct imaging of the uterus, and in turn, fibroids.
They include hysteroscopy and laparoscopy
During hysteroscopy, the doctor inserts a small telescope into the vagina to examine the inside of the womb. This allows them to easily visualize the fibromas.
Laparoscopy is a slightly more invasive procedure that allows the direct visualization of the outside of the uterus and the surrounding pelvic structures. Here, the doctor inserts a laparoscope, a tube with a small camera at one end, into small incisions that they make in the abdominal and pelvic cavities.
Treatment options
There are non-surgical and surgical methods of treatment.
Non-surgical
While there are no medications that will permanently shrink fibroids, there are drugs that can help control symptoms. These medications lower estrogen and progesterone levels, while simultaneously reducing blood flow to the fibroids. However, every case is different, and what may work for one patient may not work for another.
Doctors often prescribe birth control to reduce heavy bleeding. Short-term gonadotropin-releasing hormone agonists (GnRHa) can help shrink fibroids. They also stop menstrual flow. Long-term use of GnRHa can lead to bone loss density due to the reduced levels of estrogen. As a result, long-term use of GnRHa is supplemented with steroid hormones of estrogen and progesterone, which can safely extend the time of GnRHa use without sacrificing efficacy.
There are also several experimental treatments that are under investigation for the treatment of uterine leiomyomas.
Medicated intrauterine devices (IUD) can decrease a woman’s blood flow and thus reduce the size of her fibroids. However, this is not advised for a uterus greater than 12-weeks in size.
Some studies showed that progesterone antagonists can induce uterine shrinking and stop menstrual cycles in women with fibroids. However, this method is not available in the U.S.
The antifibrotic drug could be used to control prolonged and/or profuse blood flow in women with leiomyomas by shrinking the endometrium.
Often referred to as male hormones, synthetic androgens can also help slow or stop the growth of fibroids and relieve symptoms such as anemia and menstruation.
Finally, the French abortion pill Mifepristone can decrease the size of fibromas and reduce abdominal uterine bleeding.
Surgical
Myomectomy is the surgical removal of myomas by cutting into the uterus, followed by uterine suture repair. There are three types of myomectomies: laparotomic, laparoscopic, and hysteroscopic.
Laparotomic myomectomy is an open abdominal surgery, which gives a surgeon the full visualization necessary to remove fibroids.
Laparoscopic myomectomy is a minimally invasive abdominal surgery that is the preferred method for removing fewer than four small fibroids. This is a much more precise, difficult, and longer surgery, but is also extremely effective.
Hysteroscopic myomectomy is a minimally invasive vaginal surgery used only for small, pedunculated submucosal fibroids. This procedure does not require an incision into the abdomen.
Hysterectomy is the surgical removal of the uterus. It should only be used as a last resort. Only if the fibroids are large, diffuse, and cannot be treated any other way is a hysterectomy considered. This form of surgery is rarely needed for fibroids, and yet it accounts for ⅓ of hysterectomies in the US.
Our approach
With decades of operating experience, Dr. Seckin is highly skilled in treating cases of fibroids via laparoscopic myomectomy and uterine repair. We believe that excision surgery is the best method for removing myomas because it is the only way to remove a fibroma at its root. In cases of laser ablation, there are often small bits of myoma left underneath the tissue. Very rarely do we see the need for open, invasive myomectomy—let alone a hysterectomy—to treat fibroids.
It is important to find a surgeon who will perform a myomectomy, thus ensuring the complete removal of each underlying fibroma. Through laparoscopic myomectomy, we are able to ensure thorough removal of the patient’s fibroids, with minimal invasion. We pride ourselves on handling each myomectomy with extreme precision and attention to detail.
Patient story
Marilyn M. was diagnosed with fibroids in her early 30s after experiencing severe pelvic pain. A few years later, Marilyn was told that she also had endometriosis. After several gynecology appointments and multiple operations, Marilyn’s half-decade battle led her to see Dr. Seckin, one of the best fibroid surgeons. Read more on how Marilyn’s treatment and comprehensive laparoscopic surgery combined with hormonal supplementation medication have changed her life.
You can read more patient stories in our testimonial section.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.