Why do I have shoulder pain after endometriosis surgery?
For first-time laparoscopic endometriosis surgery patients, post-operative shoulder pain can be an alarming symptom. But patients who have had multiple laparoscopic procedures know all too well that shoulder pain, and accompanying rib and chest pain, is common. Regardless of whether you’re a first-timer, shoulder pain is common after laparoscopic surgery.
Where does this pain come from?
Your endometriosis operation was in the pelvic area, so why are you feeling pain way up into your shoulder? This is because of the CO2 gas that is used to inflate the abdomen before surgery. This gas can remain in the abdomen and irritate the diaphragm. This, in turn, can irritate the phrenic nerve, which has origins in the diaphragm and nerve endings in the shoulder.
Much of the gas will be removed towards the end of the procedure. However, residual gas can often remain, causing pressure along with the diaphragm.
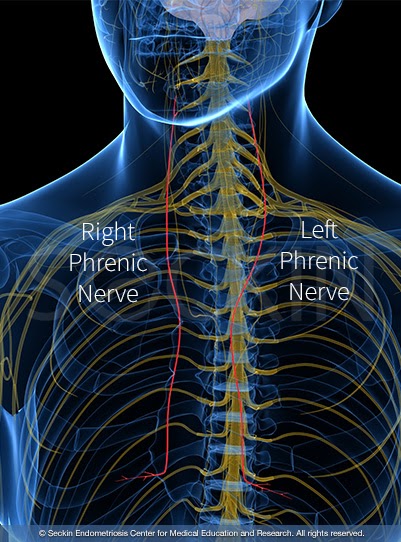
The phrenic nerve
The phrenic nerve is a nerve that originates in the neck and goes down to the diaphragm. Irritation to the diaphragm may cause a person to feel pain in the shoulder area.
How common is shoulder pain after endometriosis surgery?
Around 35 to 80% of patients who undergo laparoscopic surgery for endometriosis experience shoulder pain post-op. The pain can last two to three days or longer depending on the pain medication the patient is on. At Seckin Endometriosis Center, we do not prescribe narcotics for this very reason. Narcotics slow bowel movements following surgery. The drugs can cause constipation, bloating, further trapped gas, and can even cause an ileus (the temporary paralysis of intestines). We recommend avoiding narcotics, rotating Tylenol and ibuprofen along with Gas-X, a stool softener like Colace, and, if needed, a laxative.
Causes of shoulder pain
About laparoscopic surgery
During laparoscopy, surgeons make a small cut into the belly button, through which they insert a tube called a trocar to pump CO2 gas into the abdomen. Inflating the abdomen with CO2 gas allows the surgeon to have the best possible visibility throughout the abdomen. It also serves to put back pressure against the intestines and protect them during surgery.
Next, surgeons insert a laparoscope through the trocar. The laparoscope visualizes the inside of the abdomen. They then insert surgical instruments through other small incisions and port sites to remove any endometriotic lesions or perform any other necessary procedures.
Once the surgery is over, CO2 is released from the abdomen, and skin incisions are sewn together. However, despite best efforts to suction out all of the gas, some CO2 often remains inside the abdomen.
Treatment of shoulder pain
Gas pain in the shoulder following laparoscopic surgery can be reduced by:
- walking around, taking a hot shower, and lying on your side
- drinking hot liquids like tea and soup as well as plenty of water and fluids with electrolytes
- using nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, diclofenac, and Tylenol instead of narcotics
- taking simethicone (Gas-X) and getting your first bowel movement going with stool softeners, hydration, and laxatives (if needed or advised)
- applying heat pads to the affected area
Our approach
CO2 gas isn’t the only source of shoulder pain after laparoscopic surgery. Excess fluid or blood clots trapped in the upper abdomen and between the diaphragm and right upper liver lobe could also be to blame. Therefore, before finishing the surgery, we make sure that we remove all gas, blood clots, and excess fluid. We then perform a secondary, surgical pause before closing the patient.
This pause is crucial as we finish the procedure. We do not close the skin incision immediately. Instead, we pause for five minutes. During this five-minute recess, we place the patient in a flat, preferably reverse T-position. We call this the “head up” position. This way, all the venous blood, and gas are brought through the pelvic cavity. This decreases the pressure inside the abdomen to its normal level. We also tell the anesthesiologist to lighten the anesthesia slightly, so the patient’s blood pressure increases. We also check the excision sites for late oozing and bleeding.
After three to five minutes of recess, we re-fill the inner abdomen with gas. We then check the excision surfaces for delayed bleeding. The cause of pelvic discomfort and hematoma, solid swelling of clotted blood within the tissues will be the cause of delayed bleeding. The excision surgeon controls every site of oozing during endometriosis surgery. We keep the excision surfaces completely dry. We then suction all the excess fluid, as well as blood clots that have been accumulating. Finally, we keep the tip of our suction tube at the upper abdominal corners of the liver. This decreases gas accumulation inside the peritoneum and shoulder pain following surgery. More importantly, suctioning the blood clots under the diaphragm prevents shoulder pain that developing adhesions would otherwise cause.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.
