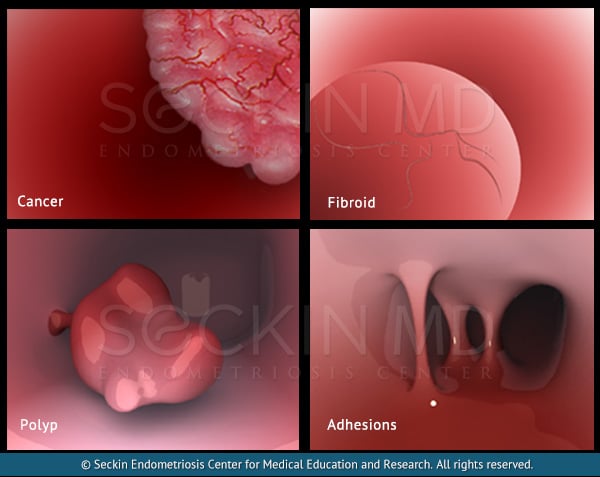
Endometriosis is the most common cause of adhesions in the pelvic and abdominal cavity. Years ago, researchers thought that the most common cause of adhesions was pelvic inflammatory disease (PID).
Endometriosis adhesions cause scarring and fibrous bands to form, which contain endometriosis glands, stroma, and inflammation. This is in contrast to more typical adhesions caused by repeated surgery, which contain only fibrous bands.
The most common endometriosis adhesions form and cause scarring within the ovaries, fallopian tubes, uterus, small intestines, and pelvic sidewall, between the bowel, rectum, and recto-vaginal septum. These “sticky” adhesions can cause the space between two organs to fill with scar tissue and inflammatory enzymes. This ultimately can lead to pain in the pelvis and abdomen. So, it is important to clearly define them, state their role in endometriosis development, and discuss treatment options for patients in their day-to-day life.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
How do they form?
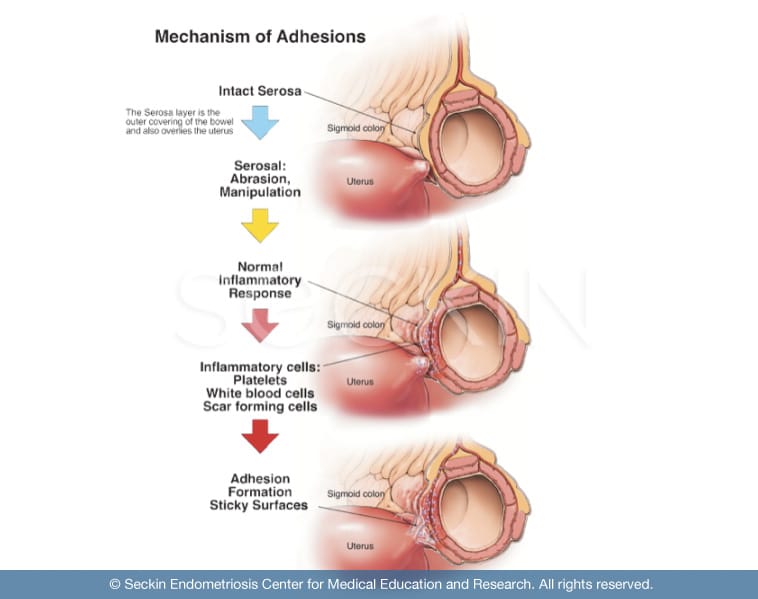
Most adhesions form in response to a tissue disturbance that triggers the body’s repair mechanism. There are a variety of factors that can trigger this including surgery, infections, and diseases such as endometriosis.
Adhesions secondary to surgery
One of the most common causes of adhesions is surgery. This occurs as a result of the body’s natural attempt to maintain homeostasis (balance).
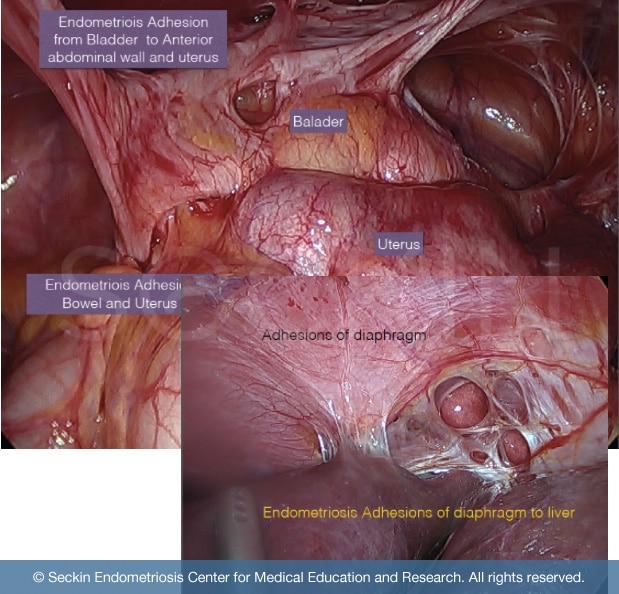
Following a C-section, it is common for adhesions to form in the bladder with a band-like tightness that spans to the anterior wall of the uterus. This can cause difficulty or pain with urination.
Adhesions can also form along the anterior and posterior uterine wall following myomectomy, even upon laparoscopic procedures. In fact, bleeding can often arise upon posterior myomectomy procedures. Therefore, it is crucial that you find a surgeon who will actively work to minimize bleeding through meticulous skill and experience. This will ensure a reduced risk for further adhesion formation and loss of blood.
Even when surgeons remove the uterus with hysterectomy, adhesions can form on the surrounding reproductive and pelvic organs. These include the ovaries, bowels, and bladder.
Surgery should only be performed as a last resort and if other treatment options are not beneficial to the patient.
The point of conducting surgery is to help the patient and relieve their symptoms. However, this does not mean that complications cannot arise and that there are no risks. Therefore, it is important to discuss with your doctor whether surgery is the right choice for you. If so, speak with your surgeon about the ways they ensure minimal risk and a minimally invasive surgical approach.
Adhesions secondary to infection
Infectious diseases can often lead to adhesions. This includes infection that causes PID and can be cause for concern, as they can increase a woman’s risk of infertility and ectopic pregnancy.
Adhesions secondary to innate pathology (i.e. endometriosis)
When we say adhesions caused by pathology, we mean those forming due to a much more serious disease. Endometriosis is just one example. Endometriosis adhesions, composed of ectopic endometrial tissue, inflammatory enzyme, and old, pooled menstrual blood, can form throughout the pelvic cavity. These can be a cause for concern as their formation can increase a patient’s chances of experiencing the symptoms of the underlying disease as well as putting them at a higher risk of infertility, bowel dysfunction, or obstruction.
Symptoms
Pelvic adhesions can cause varying symptoms. This depends on their severity and location. The most common universal symptom that adhesions can cause is pain due to pulling on nerves. This occurs as the adhesions glue organs together due to their “sticky” nature. This causes overlapping and pressure on specific nerves and tissue within the area. Other symptoms include:
- pain with deep breathing
- painful bowel movements, cramps, constipation, diarrhea, gas, bloatedness, nausea, vomiting, decreased appetite, weight loss, difficulty passing stool
- pain with intercourse or menstruation
However, physicians usually attribute these symptoms to the diseases that adhesions cause, rather than the adhesions themselves, leading to misdiagnosis or inefficient treatment.
If you are experiencing any of these symptoms, and feel that pelvic adhesions are a probable cause of your pain, you should alert your gynecologist immediately. However, remember that not all adhesions cause pain, and not all pain is due to adhesions
Endometriosis adhesions
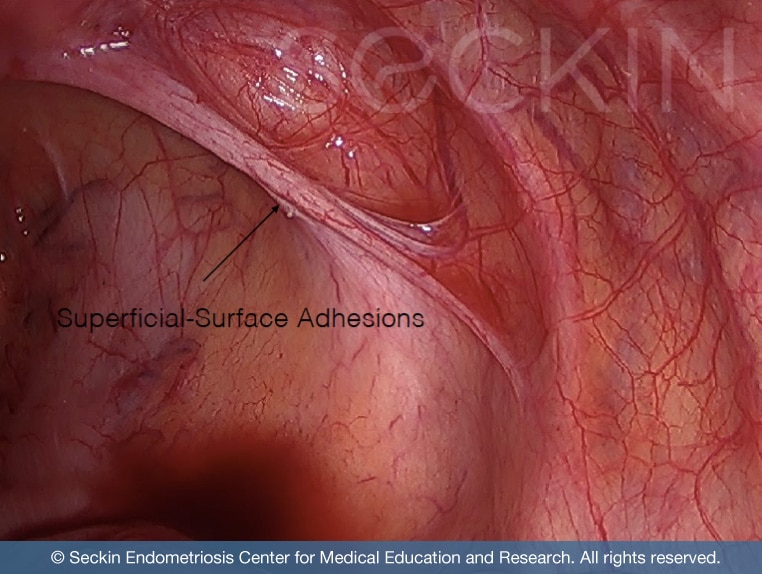
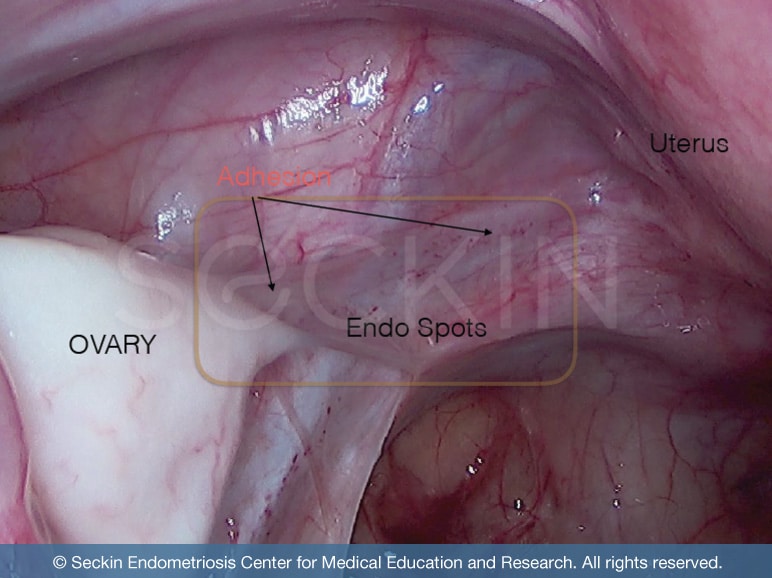
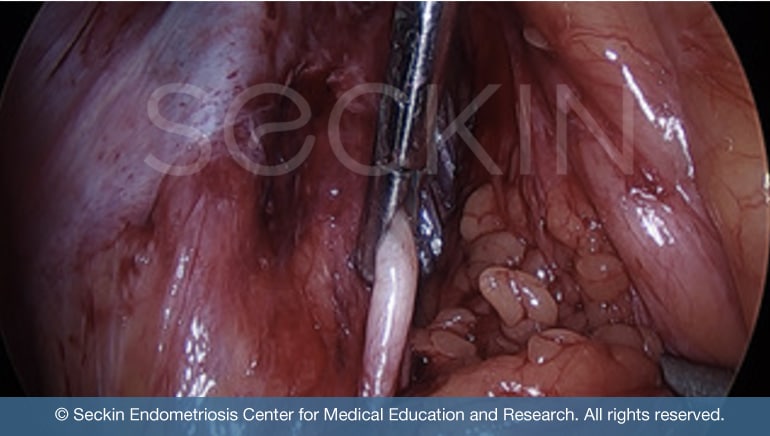
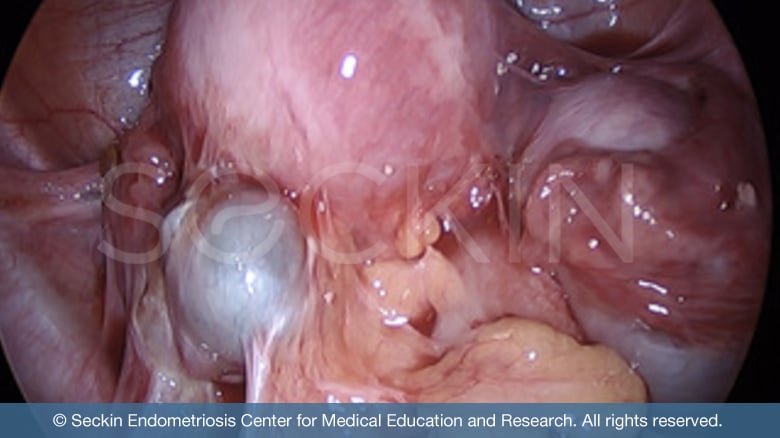
Endometriosis adhesions are unique and different from any other form of adhesions. They are often described as a sort of super glue. This is because they possess a certain “sticky” component that makes them fuse other tissues together and connect organs. This eliminates the dissection line during surgery. Normally, this space clearly separates adjacent organs. However, in the case of endometriosis, it is remarkably difficult to distinguish the line of tissue that should separate said organs. The loss of normal surgical planes can change the contour of an organ making surgery very difficult.
Endometriosis adhesions are “alive”. This means that they contain glands and stroma with endometriosis tissue within the adhesions that are reactive to estrogen. These can resemble the leakage of endometriosis material from a chocolate cyst (endometrioma). The melted chocolate-like material, which is a combination of pooled menstrual blood, inflammatory enzymes, and endometriosis tissues produced from an endometrioma fuses organs together by forming a layer of “sticky” glue-like tissue. Thus the endometriosis tissue contained within this material may be responsible for progressing into more advanced and severe adhesions that fuse organs together in extreme cases.
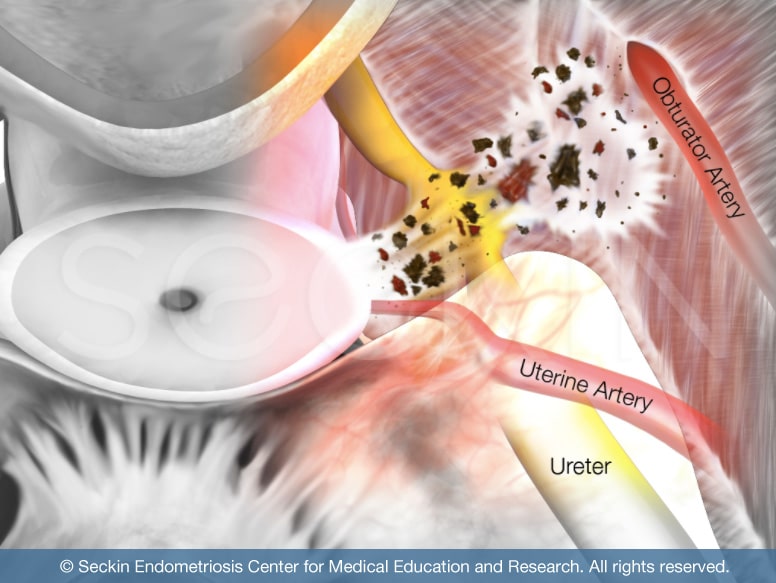
When organs are fused they cannot function well. This leads to issues such as rectal constriction causing constipation or retroperitoneal infiltration, leading to retroperitoneal fibrosis. It can also cause severe sharp pain with intercourse or an inability to tolerate it with a deep pulling sensation. Other inner anatomical abnormalities that can arise from adhesions include ureter and bowel blockages and deep cul-de-sac scarring and obliteration. In this sense, endometriosis adhesions are unique in comparison with the adhesions that form due to surgery.
What are the steps of progression?
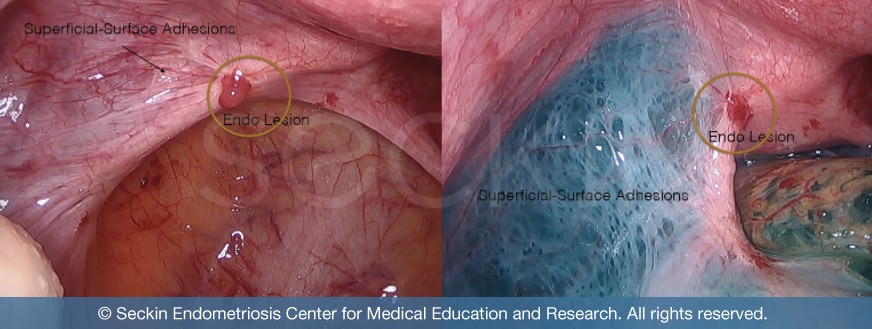
During early endometriosis, the primary organ affected is the peritoneum (the lining of the abdomen). However, the exact cause leading to the progression of stage 1 endometriosis and further development is not clear. While there are several theories, ranging from Sampson’s theory of retrograde menstruation to the stem cell theory of endometriosis, it is likely that there may not be one singular cause. Instead, a multitude of mechanisms likely works alongside one another. Either way, small patches and lesions of endometriosis tissue within the peritoneum are a common anomaly in cases of early endometriosis development.
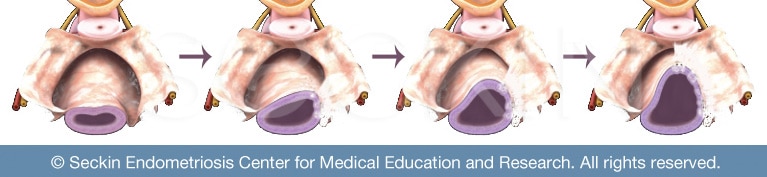
In more severe cases of endometriosis, it is not uncommon to find endometriosis tissue on the ovaries. This collection of endometriosis can cause the formation of an ovarian cyst called an endometrioma. This also consists of pooled menstrual blood and inflammatory enzymes. This “chocolate cyst,” termed after the brown serous fluid it consists of, is then susceptible to leakage during menstruation and subsequent further spreading of endometriosis within the pelvic cavity. This material can then go on and form adhesions throughout the pelvic cavity.
When the leakage of this material spreads throughout the pelvic cavity, endometriosis adhesions grow and spread. These adhesions serve as a “glue” that holds inflamed pelvic organs in place. They can ultimately result in extreme cases like frozen pelvis. This can cause symptoms such as chronic pelvic pain, killer cramps, and pain with sexual intercourse.
Where do endometriosis adhesions commonly form?
Most commonly, endometriosis adhesions adhere to the pelvic cavity due to their uterine origin. Below is a few common organs within the pelvic cavity where endometriosis adhesions adhere to:
- uterine muscle layer or serosa layer (adenomyosis)
- fallopian tubes
- ovaries (endometrioma)
- bladder
- ureter
- cul-de-sac (both posterior and anterior)
Adhesions also commonly affect organs within the abdominal cavity, particularly in cases of bowel endometriosis, which is seen in nearly one in every five endometriosis patients.
Common sites within the abdominal cavity that endometriosis adhesions stick to include:
- peritoneum
- rectum
- colon (large intestine)
- appendix
- ileum (the final section of the small intestine)
In rare instances, endometriosis implants and adhesions can incorporate a variety of other locations, which include:
- cervix (excluding the endometrial layer)
- vagina
- nerves
- lungs
- brain
How can endometriosis lead to retroperitoneal fibrosis?
Retroperitoneal fibrosis is when fibrous adhesions form in the space behind the peritoneum. This can often be due to endometriosis adhesions infiltrating the peritoneum and spreading through the wall.
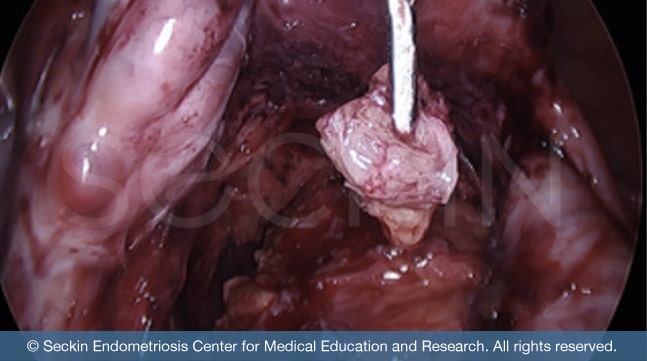
When this occurs, the adhesions can continue to spread and are often associated with the involvement of the ureter and deep nerves. This will cause symptoms such as neuropathy (pain due to nerve damage), particularly in the legs and below the lower abdomen. In these cases, it is important that these adhesions are meticulously removed through “cold” excision surgery, using minimal to no electrical energy. In this way, the pelvic and abdominal cavity is repaired/restored and reconstructed.
Diagnosis
Adhesions are not a formal medical diagnosis. However, we strongly recommend that you see a doctor if you experience these symptoms.
The underlying pathology cannot be identified with any simple form of a diagnostic exam. In order to do so, a surgeon must take a biopsy sample during laparoscopic surgery. He or she then sends this specimen to a pathology lab, where a pathologist will observe it under a microscope and provide a report with an official diagnosis.
Treatment
Doctors must diagnose and treat adhesions medically. Treatment can vary depending on the severity and location of the adhesions, as well as the bigger issue that the adhesion is causing.
Non-surgical treatment
Because many adhesions do not cause any symptoms at all, surgery does not become necessary unless in case of an emergency. In fact, they often improve without surgery. Even in instances of mild pain, a physician will more commonly treat the symptoms than go to such extensive measures as surgery.
Diet
Diet certainly cannot rid a patient of their pelvic and abdominal adhesions. However, it can help play a role in symptom relief. Because abdominal adhesions can implant on the bowels, they often mask themselves as other disorders like irritable bowel syndrome (IBS). These can include nausea, constipation, small bowel production, and bowel obstruction. So, it can be helpful to adopt lifestyle and dietary changes, such as the FODMAP diet that can help relieve such symptoms.
Surgical treatment
The two most common forms of surgically treating pelvic and abdominal adhesions are laparoscopy and laparotomy. These differ primarily in terms of invasiveness.
A laparotomy is an open surgical technique where the surgeon makes a large incision from the navel (belly button) down to the abdomen. This gives them full access and visualization of the abdominal and pelvic organs. Laparotomy is a much more invasive technique and thus presents more risk of a difficult recovery. Therefore, in most cases, laparoscopy is the preferred form of surgery. However, only an experienced and skilled surgeon can perform this. It is important to remember that surgery in itself can cause adhesions. However, there are few proven methods to prevent this.
Our approach
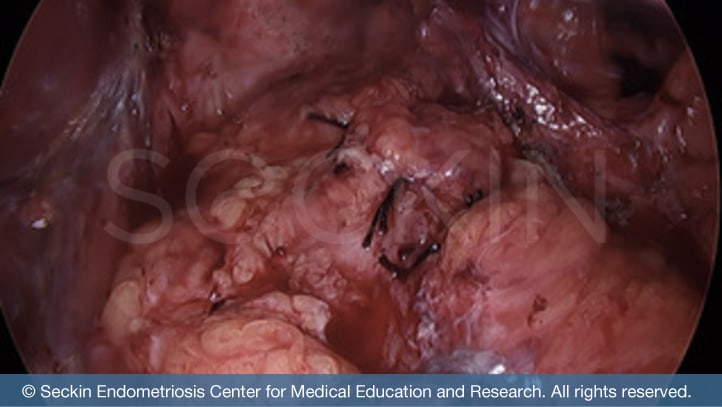
At Seckin Endometriosis Center, we are committed to performing laparoscopic surgery. We believe that a patient’s best chance of healthy recovery and symptom relief is through minimally invasive surgery. Thus, we perform excision surgery to remove all suspected adhesions as an initial step in surgery. Additionally, we are able to better view and thus remove endometriosis adhesions through our patented ABC technique. Our method differs from traditional adhesiolysis. We firmly believe that both endometriosis adhesions and their surrounding scar tissue must be meticulously removed through excision. This ensures that adhesions are fully removed individually, including the underlying tissue beneath the surface. After decades of training and experience and with a team approach, we are able to provide a highly thorough and productive surgery, which includes repairing, reconstructing, and restoring the organs that were operated on.
If you or your doctor feel that you could have pelvic adhesions and have had constantly recurring pain, please feel free to call us to discuss your case.
Pelvic adhesions due to endometriosis can be a very grueling condition to endure, and even more so to treat. We have worked tirelessly to improve upon our techniques to ensure that our patients receive the conservative and definitive surgery that they both need and deserve.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.