In every menstrual cycle, the ovaries go through cystic changes. As menstruation progresses, a signal to the brain causes a series of eggs in the ovaries to be selected for ovulation. Only one of these will hatch. Prior to hatching, a follicle develops. The size of this follicle is about 2-3 cm and it is called a physiological ovarian cyst. This is a natural phenomenon in the menstrual cycle for every woman.
Beyond this, any pouch or sac filled with fluid or other tissue that formed on the ovary is also an ovarian cyst. In general, an enlargement of the ovary cyst beyond 4 cm can cause persistent discomfort. It would, therefore, alert a patient and their doctor of a possible problem. It is critical to follow these ovarian cysts to rule out possible conditions such as endometriosis or ovarian cancer. Nevertheless, cysts are most often benign. Even when they are abnormal, rarely do they require removal of the ovaries (oophorectomy).
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Why are ovarian cysts difficult to identify?
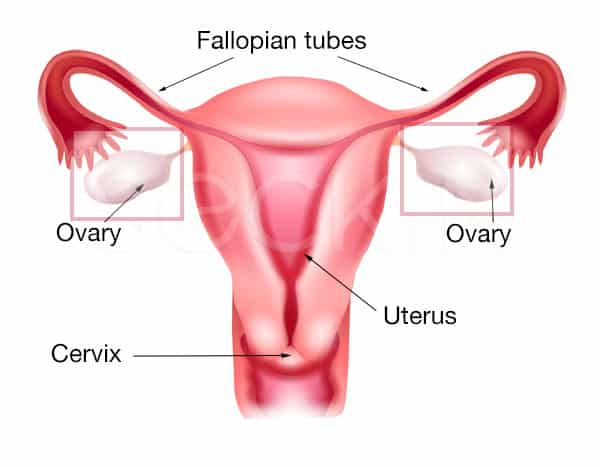
Just as men have two testicles, females have two ovaries. These are the site of possible ovarian cyst development. However, while men can clearly see their reproductive organs, female anatomy presents a much more difficult challenge as the ovaries are within the pelvic cavity. On top of this, typical ovarian cysts are a normal part of a woman’s ovulation cycle. Because of these facts, ovarian diseases, such as ovarian cysts can be much trickier to diagnose. Nevertheless, painless imaging techniques such as sonography can help provide a presumable diagnosis of the type of ovarian cyst a patient may have.
Causes of ovarian cysts
To understand how ovarian cysts form, it is first important to know how a healthy egg leaves the ovary. Before this can happen, a follicle must form. Follicles are small, fluid-filled sacs that are “normal cysts”. They create a protective environment in which an egg can properly develop. Upon ovulation, the follicle breaks, and a mature egg enters the fallopian tubes. The remaining hemorrhagic fluid leaks out of the ovary. This leakage, along with follicle development and breakage, is a normal process in the production of healthy eggs. However, it does present one area where abnormal ovarian cysts can arise.
Follicle abnormalities can occur in several different ways. First, there are cases where the follicle does not break. In turn, the fluid remains in the tightly packed sac, forming a follicular ovarian cyst.
Ovarian cysts can also arise after ovulation when the egg is released and the follicular breakage reforms to make the corpus luteum. The normal lifespan of this structure is 14 days following ovulation. However, there are situations when the corpus luteum does not dissolve and in turn, corpus luteal cysts arise. Blood and other forms of bodily debris such as ectopic endometrium or even neoplastic tissue also play a role in the formation of several other forms of ovarian cysts. The female reproductive system is incredibly complex, and it is crucial for each step to occur in a coordinated manner.
Polycystic ovarian syndrome (PCOS) is a hormonal disorder that causes small, benign cysts to arise throughout the ovaries. While these cysts may not be harmful, they often lead to further hormonal imbalances. This can cause symptoms such as irregular periods, acne, and infertility.
Classifications of ovarian cysts
There are many different forms of ovarian cysts that can arise, both physiologically and pathologically. Below are a few of the most common forms of ovarian cysts.
Follicular cysts
These are ovarian cysts that form when the follicle containing a developing egg does not break. They are most often painless and harmless and resolve after a few menstrual cycles.
Corpus luteal cysts
When the corpus luteum does not dissolve according to the right timeline a corpus luteal cyst will form. The right timeline is 14 days after ovulation without fertilization and 14 weeks in the presence of pregnancy. Oftentimes, the internal tissue of these cysts undergoes necrosis (uncontrolled cell death). This causes bleeding to stay within the cyst itself. When this happens the cyst is termed a hemorrhagic corpus luteal cyst.
These cysts can easily be confused with an endometrioma, which is a detrimental mistake. Usually, hemorrhagic cysts are benign cysts that will go away on their own within a few weeks, with no treatment. However, endometriomas can be highly dangerous. This is because they can lead to the spreading of endometriosis, as well as ovarian torsion (a major emergency that should be treated right away). It is invaluable to make the distinction between these two forms of cysts.
Endometriomas
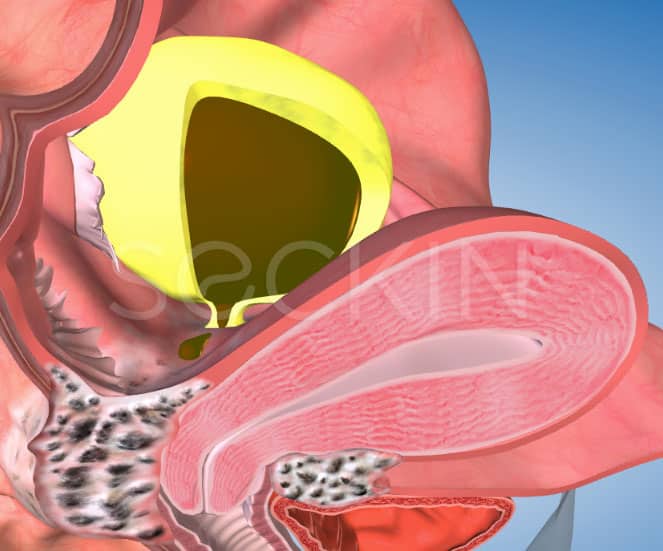
Also known as “ chocolate cysts,” these ovarian cysts will contain fragments of endometriosis tissue and possible retrograde menstruation blood that ultimately pools together and degenerates, making a chocolatey brown serous fluid.

Dermoid ovarian cysts (teratomas)
These cysts will typically develop when a woman is at her most fertile. It will contain hair, fat, or any other form of abnormal tissue. They can usually take on both a solid and cystic form and can cause pain, infection, rupture, and even cancer in some cases.
About 15-20% of dermoid cysts are bilateral, meaning they grow on both ovaries, with less than 3% being malignant (cancerous). It is thus highly advised to surgically remove a dermoid ovarian cyst. An experienced laparoscopic surgeon must perform ovarian surgery for dermoid cysts to ensure that the dermoid contents do not spill into the peritoneal cavity. Depending on their size, ovaries need to be reconstructed skillfully, without resorting to the use of electrosurgery, which can affect ovarian blood supply and eliminate ovarian reserve by coagulating healthy eggs.
Cystadenoma
This benign ovarian tumor usually develops on the outside of the ovary. It can be full of mucous (mucinous cystadenoma) or of a clear yellow serum (serous cystadenoma). They can grow to be very large but are most often not harmful. However, research has shown that serous cystadenomas have more of a tendency to develop into cancer.
What is ovarian torsion?
When ovarian masses arise, such as abnormal ovarian cysts, one of the common complications that can occur is ovarian torsion. When the ovarian cyst is large enough, it causes the ovary to rotate and twist around its root. This ultimately cuts off the ovarian blood cell line. Fallopian tube torsion can also arise in congruence with ovarian torsion. This is one of the primary reasons why abnormal ovarian cysts can cause symptoms such as pelvic and lower abdominal pain, along with nausea and vomiting. However, in the case of ovarian torsion causing a lack of blood supply to the ovaries, the pain will be excruciating as the ovaries are at risk of “dying.”
Severe ovarian torsion is a medical emergency due to excruciating pain and the possible loss of ovarian function. In the emergency department, surgeons use laparoscopic detorsion, which has a 90% success rate of saving ovarian function. You should rush to the hospital if you have a history of pathological ovarian cysts and your symptoms become agonizingly painful.
Are ovarian cysts and pelvic masses the same thing?
Pelvic masses are abnormal growths in the pelvic cavity. They can be a growth or tumor in the ovaries, uterus, or any pelvic organ. Many ovarian cysts such as cystadenomas, dermoid cysts, and endometriomas are all examples of pelvic masses that can arise in the ovaries. However, fibroids can also be considered pelvic masses, and they normally occur in the uterus. Thus, ovarian cysts can usually be classified as pelvic masses, but the same is not true for the opposite.
Ovarian cysts and endometriosis
How can endometriosis lead to ovarian cyst development?
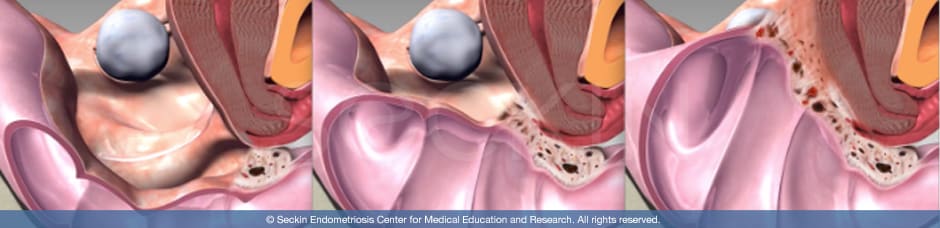
Endometriosis is one known cause of abnormal ovarian cysts, specifically endometriomas. One of the most common locations for ectopic endometrial cells to grow is the ovaries. This occurs when menstrual blood carrying sloughed off endometrial tissue moves backward through the fallopian tubes to the ovaries. The endometriosis tissue then accumulates and grows inside the ovary, eventually forming an endometrioma. This newly implanted endometriosis scar tissue will then be able to have its own “mini periods”. Here, the said lesion will begin to bleed and possibly slough off even more endometriosis tissue. The combination of these fragments of endometrial tissue, old thickened blood, and inflammatory enzymes combine together within the ovary to create an endometrioma or chocolate cyst.
How can endometriosis in the form of an endometrioma spread?
The endometriosis scar tissue that makes up a chocolate cyst will have its own “mini period,” causing blood and additional endometrium to slough off from the cyst. Therefore, endometriomas are likely to leak into other areas within the pelvic and abdominal cavity. This is one of the primary ways in which deep infiltrating endometriosis develops. When this occurs, adhesions can form in areas outside of the ovaries and spread in diffuse areas such as the peritoneum, cul-de-sac, and intestines. When this occurs, symptoms of pelvic pain, heavy bleeding, painful sex, nausea, vomiting, and cramping can often worsen. In rarer cases, the chocolate cysts can even rupture, causing the contents to spill out and lead to severe, deep infiltrating endometriosis that develops into a frozen pelvis. This is why it is important to seek an endometriosis specialist who can surgically remove endometriomas to ensure that the disease does not spread and worsen.
Why should a patient be concerned about endometriomas?
While the average ovarian cyst does not need much more than routine check-ups, and endometrioma does. This is due to four reasons.
First, there is a high possibility that endometriosis is spreading if the cyst is an endometrioma. Endometriomas will often leak into the pelvic cavity and cause deep infiltrating endometriosis. This can then spread to the rectum, bladder, and bowels. Ovarian endometriomas thus appear to be markers of more extensive pelvic and intestinal disease.
Exclusive endometriomas occur only in 1% of endometriosis cases. The remaining patients have extensive pelvic or intestinal endometriosis along with ovarian endometriosis. An endometrioma can also rupture, causing its contents, including both endometriosis scar tissue and old degenerative blood, to spill into the pelvic cavity. This can cause aggravated symptoms. It can also lead to the most serious classification of endometriosis: stage IV endometriosis with a frozen pelvis. Thus a ruptured endometrioma is a huge concern and is why a patient should consider surgery.
Another concern is the risk of ovarian torsion. If the ovary gets large enough due to inflammation and cyst growth, it will begin to turn on itself. An ovarian cyst larger than 4 cm in diameter has a greater chance for torsion than those that are smaller.
Last, research has shown that patients with ovarian endometriosis or endometrioma have a greater risk of developing certain types of ovarian cancer. These include clear cell ovarian cancer, low-grade serous ovarian cancer, and endometrioid invasive ovarian cancer. It is crucial for patients to seek an early diagnosis if they are concerned about endometrioma.
What are “kissing ovaries?”
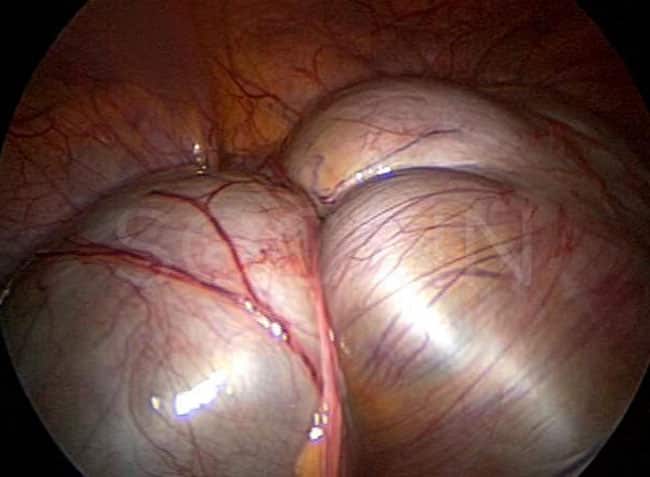
Endometriomas can be as small as a quarter or as large as a watermelon. When endometriomas and adhesions continue to grow and involve both ovaries, the ovaries can become so large and inflamed that they nearly touch each other. Endometriomas with such close proximity to one another are termed “kissing ovaries.” This condition is easily visible through vaginal sonography. It can be an indicator as to whether or not the patient has a mild or severe case of endometrioma development.
Are ovarian cysts and endometriomas the same?
While endometriosis can be the cause of developing ovarian cysts, not all ovarian cysts are caused by endometriosis. There are several classifications of ovarian cysts, and endometrioma is just one of them. Nevertheless, this is an important distinction to make as oftentimes a doctor may diagnose their patient with an ovarian cyst. This is actually a very vague diagnosis.
Keep in mind that an ovarian cyst can mean anything from a benign follicular cyst to a highly concerning and still developing endometrioma. Therefore, it is very important to consult a gynecological specialist who can differentiate between these nuances that ultimately call for a completely different plan as to whether or not to monitor the cyst. This distinction can be the difference between a presumptive misdiagnosis of a benign follicular cyst, which can resolve on its own, versus a growing endometrioma, which is an indicator of endometriosis and possible deep infiltration of endometriosis that requires surgery.
Symptoms of ovarian cysts
Most often, ovarian cysts will present no symptoms as they are small and benign. Symptoms can also vary depending on the type of ovarian cyst. Nevertheless, in cases of abnormal and potentially harmful ovarian cysts, the following symptoms can arise:
- irregular and painful menstrual bleeding and periods (dysmenorrhea)
- pelvic pain, especially during the period
- pain with intercourse (dyspareunia)
- nausea, vomiting, diarrhea, or bloating
- bladder and bowel pain and dysfunction
- lower back pain that can radiate to thighs and legs
- fatigue
Diagnosis of ovarian cysts
There are multiple ways in which doctors can diagnose an ovarian cyst. However, the best way to presumptively do so is through sonography, which is ideally performed through the vagina as opposed to the abdomen.
Transvaginal ultrasonography
Here, your doctor will insert the ultrasonograph into your vagina in order to produce real-time images on a monitor. Through these images, he or she will be able to assess whether or not you have an ovarian cyst. He or she will also be able to tell the shape, size, location, and components that make up the cyst. This is key in determining whether the cyst is full of fluid, solid, or a mix of the two. These key distinctions will ultimately determine whether or not your surgeon will operate on you.
Magnetic resonance imaging (MRI)
MRI is a key diagnostic tool that can help evaluate pelvic pathology. Before any surgery, a physician may ask their patient to receive an MRI in order to obtain clear imaging of the ovaries. This provides the doctor with a greater understanding of the size, severity, and extent of the ovarian cyst.
CAT scan
A computerized axial tomography (CAT scan) can be highly useful in determining whether an ovarian cyst is abnormal. It is primarily used to detect malignancy and abnormal ovarian growth that causes invasion of adjacent organs, lymph, and blood vessels. Thus, a CAT scan can often rule out any immediate emergency or need for surgery.
Laparoscopy
Laparoscopy is a minimally invasive technique that uses a laparoscope in order to clearly visualize the ovaries and any cysts that may be present. Surgeons perform this technique in the operating room while the patient is under anesthesia. It is often referred to as minimally invasive surgery (MIS). The number of incisions and incision sizes can vary from one surgeon to another depending on their experience, skill, and the method they use.
Blood tests
Cancer antigen (CA) 125 is a protein that is often measured in blood tests for cases of ovarian cancer. Research has shown that CA 125 levels are significantly high in moderate or severe endometriosis compared to minimal or mild disease. However, the low sensitivity of this test poses a limitation in its clinical use for endometriosis. Serial CA125 determinations may be useful to predict the recurrence of endometriosis after therapy.
Treatment of ovarian cysts
Medical treatment
One of the first measures doctors will take in attempting to treat abnormal ovarian cysts is to prescribe medication. Of these, birth control is the most common. By prescribing oral contraceptives, the doctor is attempting to prevent ovulation, and thus the further development of ovarian cysts. Oral contraceptives may be useful in relieving a patient’s symptoms. However, they do not cause pre-existing dangerous ovarian cysts, such as endometriomas or cystadenomas, to disappear. In other words, medication will not remove the abnormal cyst itself. However, medications do aid in relieving the symptoms that the cyst causes.
Ovarian cyst surgery (ovarian cystectomy)
Ovarian cystectomy is the surgical removal of ovarian cysts where the function of the ovaries is intact. This is made possible by laparoscopic surgery, which is considered the “gold standard” for both visualizing and treating abnormal ovarian cysts. By making several small incisions into the abdomen and pelvis, a surgeon is able to insert a laparoscope in order to clearly visualize and operate on a patient’s ovaries, fallopian tubes, and surrounding reproductive organs. However, it is important to find a surgeon who will not only perform minimally invasive laparoscopic surgery in order to properly remove an ovarian endometrioma, cystadenoma, etc., but will also carefully preserve ovarian function, and will only remove the ovaries if necessary.
Our approach
We strongly believe that diagnosing and treating ovarian cysts must be handled with great care. We believe the most important element of successful ovarian surgery is ensuring the patient that we will only remove her ovaries if absolutely necessary. This occurs rarely.
Second, we make sure we preserve the ovarian cortex, which houses a woman’s developing eggs. In order to do so, we conduct our surgeries very meticulously. We adhere to the principles of microsurgery, which clearly state the great need for fine tissue handling. This means not using electricity or cauterizing the ovary, or “cooking” the ovaries. Our goal is to ensure that our patients have as few complications and risks as possible. This is why we abide by the technique of “cold” excision, meaning surgical removal of abnormal cysts without electricity.
We also ensure the preservation of ovarian functionality following the removal of ovarian cysts by conducting ovarian reconstruction surgery. Just as a plastic surgeon reformats and recreates tissue, we look to do the same with the ovaries to preserve their functionality.
Finally, we suspend the ovary from the pelvic wall. This ensures that it does not “stick” to other tissue, or the other ovary, following surgery.
By conducting a very precise, careful ovarian laparoscopic surgery technique, on top of assessing patients pre-surgery through transvaginal ultrasonography and MRI, we ensure that we handle every case with the care and patience that it deserves. Proper diagnosis and classification of ovarian cysts is a very tricky subject and only the most experienced ovarian cyst specialists should take it up. We like to combine our world-renowned expertise with our unique philosophy of personal care. Not every case is the same and, therefore, we listen to every patient.
Patient story
Candie, an actress, and musician had ovarian cysts in each of her ovaries after experiencing horrible symptoms such as killer cramps, painful ovulation, back pain, constipation, nausea, and vomiting. Initially, doctors told her that her symptoms were “in her head.” But Candie went on to seek surgery—only for a proclaimed “endometriosis specialist” to operate on her. Candie was able to find us and receive the surgery that she needed. Learn about Candie and her story and her successful endometrioma and surrounding endometriosis removal surgery, and remember her triumph can be yours too.
You can read more stories of patients with ovarian cysts in our testimonial section.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.
