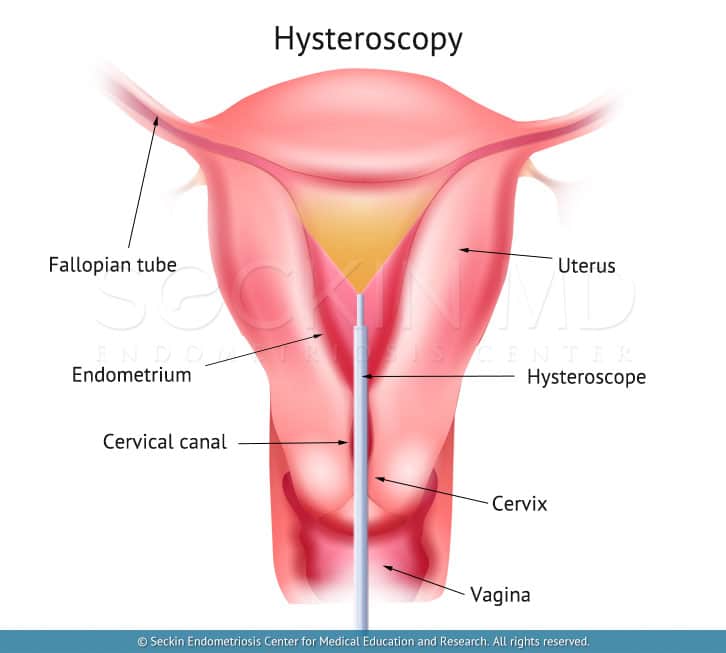
A hysteroscope is a thin telescope that a surgeon inserts into the uterus via the natural orifice (vagina through the cervix) to visualize the endometrial cavity, as well as the tubal stia, endocervical canal, cervix, and vagina. The name of the procedure that uses a hysteroscope is hysteroscopy.
Patients may need local anesthesia when the procedure takes place in the office setting. Procedures requiring only diagnostic evaluation of the cavity, and minor procedures of endometrial biopsy and polyp removal, should not require a hospital setting. However, an operative hysteroscopy for the shaving of fibroids (as with myosure and intrauterine septum resection) requires general anesthesia. Specialist hysteroscopic surgeons should perform these procedures due to potential unintended consequences.
What are the indications?
Hysteroscopy has many indications. These are listed below.
- diagnosis and treatment of abnormal uterine bleeding (diagnostic hysteroscopy procedure)
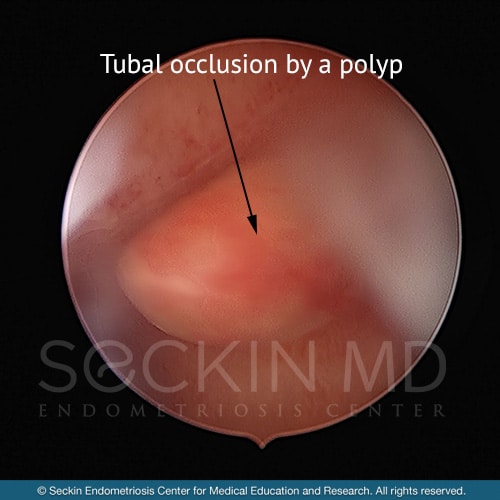
- endometrial polyps
- intracavitary fibroids
- intrauterine adhesions caused by infections or previous surgical procedures
- diagnosis and/or treatment of uterine anomalies (eg, uterine septum, arcuate uterus)
- retained intrauterine devices or other foreign bodies
- insertion of intrauterine tubal contraceptive devices
- endocervical lesions
What is the role of hysteroscopy during endometriosis surgery?
According to the Sampson theory (which researchers believe to be the most common theory for endometriosis), the cells causing endometriosis lesions are coming from the endometrial cavity. Knowledge of the endometrial cavity is therefore essential. Endometriosis patients tend to bleed more than other women, and most have cavitary abnormalities including endometrial polyps, uterine structural abnormalities, and Mullerian anomalies.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
According to our unpublished data, out of 941 patients who had endometriosis surgery with us and a hysteroscopy, 645 (68%) had some kind of uterine abnormality including uterine structure abnormalities such as cornual funneling, midline prominence, arcuate uterus, fibroids, septum, etc, and 38% of these abnormalities were arcuate uteruses.
Types of hysteroscopy
Office hysteroscopy
Office hysteroscopy takes place in the physician’s office. Its narrow and thin camera allows easy access to the endometrial cavity. Ambulatory settings are ideal for patients, as they are time-saving compared with operating room procedures, and should be used whenever feasible. But an office hysteroscopy may fail because of pain, cervical stenosis, and poor visualization.
Operative hysteroscopy
An operative hysteroscopy procedure (or procedure hysteroscopy) takes place in the operation room. It requires anesthesia because of the need for cervical dilatation and the timelapse of the procedure. Operative hysteroscopy will solve most cases that require uterine intervention. These include:
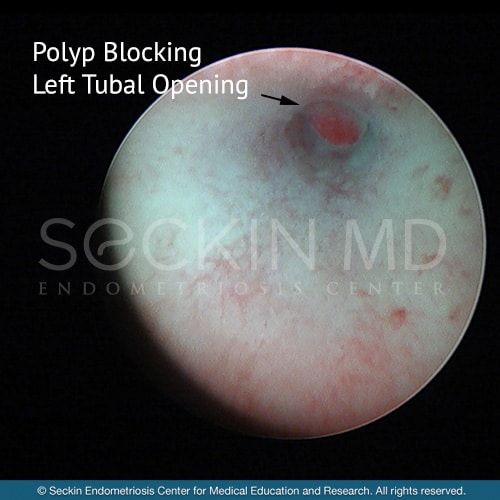
- large uterine polyps
- cavitary fibroids
- long uterine septums
- intracavitary adhesions
Recovery after hysteroscopy
Most patients experience postoperative cramping or light bleeding and some complaints of vaginal discomfort, which mostly ease in 15 minutes. Paracetamol or nonsteroidal anti-inflammatory drugs like Advil, Tylenol, or Brufen are usually adequate for postoperative pain control, if necessary.
Patients can resume their daily activities within 24 hours. At Seckin Endometriosis Center, we see patients for a follow-up visit seven to ten days after the operation to assess any further complications and review results.
Risks and complications
Complications from hysteroscopy are rare but could be serious if not managed by an experienced doctor. They include:
- uterine injury
- anesthesia-related complications
- infections
- excessive fluid absorption due to the uterine distention media
- hemorrhage
Infertility
Uterine abnormalities may prevent implantation of the embryo to the endometrial cavity. All abnormalities should be evaluated for a patient who desires fertility. The uterine anomalies that are most common during hysteroscopy that may prevent implantation are adhesions, septa, polyps, cavitary fibroids, anomalies of the cervical canal, and lesions of the tubal cornual channels. According to literature, most of the patients with cavitary lesions profit from hysteroscopic treatments, and almost 65% achieve pregnancy.
Hysteroscopy FAQs
Is a hysteroscopy painful?
Most patients experience postoperative cramping or light bleeding and some complaints of vaginal discomfort.
What intrauterine conditions can be treated with hysteroscopic surgery?
The following conditions can be treated by hysteroscopy:
- endometrial hyperplasia
- endometrial cancer
- large uterine polyps
- cavitary (subserosal) fibroids
- long uterine septums (uterine subseptus)
- bicornuate uterus
- unicornuate uterus
- intracavitary adhesions
- intracavitary foreign bodies
- embedded IUD
- perforating IUD with lost string
- any abnormality present inside the uterine cavity
What is the recovery time after a hysteroscopy?
Hysteroscopy is a one-day surgery. You will start feeling better just after the procedure and could get back to your daily routine the day after the surgery.
What is a hysteroscopy D&C?
If you are having heavy periods and are at risk of having uterine malignancies, you need to have an endometrial sampling. After evaluating the endometrial cavity to visualize the reason for your abnormal bleeding with hysteroscopy, a dilation and curettage (D&C) of the endometrial cavity is usually made and the sample is sent to the pathology department for histologic diagnosis.
Do I need anesthesia for a hysteroscopy?
Office hysteroscopy does not require anesthetics but if you need to have an operative hysteroscopy for your lesions you will need sedation because of the need for cervical dilatation and the timelapse of the procedure.
Will a hysteroscopy delay my period?
Your hormonal system will be working normally after the hysteroscopy. However, if you also have had endometrial sampling, your menstruation might be late because the endometrial lining that peels off due to menstruation every month would be collected for sampling on your hysteroscopy procedure.
What are the risks of hysteroscopy?
Complications from hysteroscopy are rare but could be serious if not managed by experienced doctors. They inlcude uterine injury, infection, hemorragia, and excessive fluid absorption caused by the uterine distention media.
Can a hysteroscopy detect cancer?
The most common way to detect endometrial cancer is with D&C. However, if cancer is present on a uterine polyp, a hysteroscopy is the perfect way to see and resect it.
How much does hysteroscopy cost?
The cost of hysteroscopy can vary. Please book a consultation with our practice for more detailed information.
Our approach
At Seckin Endometriosis Center, our specialist surgeons use hysteroscopy to inspect the uterine cavity. Instead of using the old-fashioned blind procedure of D&C, hysteroscopy is a minimally invasive visual approach for the diagnosis and treatment of common gynecologic problems such as abnormal uterine bleeding, uterine abnormalities to treat fibrosis, polyps, adenomyosis, endometrial hyperplasia, and heavy menstruation with clots. Hysteroscopic evaluation of the uterine cavity is the gold standard in the investigation of miscarriages, early pregnancy loss, and evaluation of infertility.
Endometriosis surgery should always start with an evaluation of the endometrial cavity by hysteroscopy. D&C is a touch-and-feel blind procedure. Hysteroscopy has largely replaced this procedure as the current standard of accepted practice
The best time to perform hysteroscopy is immediately after your period, or in the early follicular phase. The increased endometrial thickness would impair visualization other times during the cycle. Office hysteroscopy should always take place at the early follicular phase to obtain optimal visualization. Diagnostic hysteroscopy may be combined with laparoscopy and therefore take place in the luteal phase of the menstrual cycle, but care must be taken to avoid abrading the endometrium during the procedure, causing unnecessary trauma.
Our best approach is the “see and treat” technique in an advanced operative room with general anesthesia unless the patient prefers otherwise.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.