Frozen Pelvis is the most extensive form of advanced endometriosis, encompassing the ultimate forms of deep infiltrative endometriosis (DIE). This aggressive form of the disease is inclusive of all extreme endometriosis presentations plus unusual deep infiltrative attachments to outer limits of pelvic ligaments, nerves, and muscle tissues. Frozen pelvis can be partial or total and is synonymous with “end-stage endometriosis” or “terminal endometriosis” in the pelvis.
When frozen pelvis occurs, deep fibrotic nodules and deeply infiltrative endometriosis replace pelvic soft tissues with high-density fibrosis. Pelvic organs soon become firmly fixed to pelvic bones, making them immobile or “frozen,” comparable to the way ice feels.
Endometrial tissue can implant and invade any tissue of the body. However, it most frequently found in the peritoneal cavity of the pelvis. The peritoneum is the thin membrane that covers the uterus, ovaries, bladder, ureters, pelvic sidewalls, and bowel.
Causes of frozen pelvis
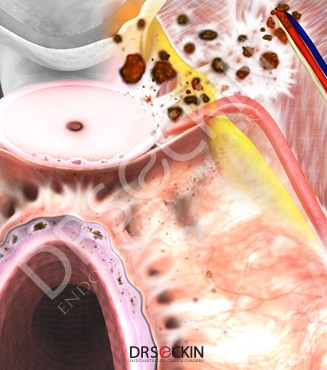
Endometrial implants are tissue similar to the one that lines the inside of the uterus. It is, therefore, affected by and subjected to a similar reaction to estrogen and progesterone fluctuations, which is to bleed. In other words, mini-menstruations occur at these implantation sites upon hormonal changes that normally cause a woman to have a period. Unlike a period, however, the menstrual blood shed from these lesions becomes trapped in the peritoneal lining.
The immune system then initiates a “fight” to clear this debris. The resulting struggle causes inflammation at the cellular level. Gradually, increased scarring, also known as adhesions take place. These adhesions can “glue” internal organs together. They can also wrap around organs and form web-like structures from organ to organ. Or they can attach to the lining of the abdomen. When a surgeon visualizes the peritoneal cavity and sees adhesions stretching from the ovary to the tubes, the pelvic sidewalls, and the cul-de-sac, they will understand that there may be more serious problem. These adhesions may extend to deeper tissues, involving the nerves, lymph nodes, and/or muscle layers of organs. When the adhesions dig deeper, they harden the soft tissues and organs in the pelvis. So what started as an early peritoneal implant becomes a total rock-like tissue due to fibrosis.
What conditions cause frozen pelvis?
- Endometriosis
- Cancer
- Pelvic inflammatory disease
- Radiation treatment
- Previous surgery (especially myomectomy)
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Symptoms of frozen pelvis
A patient with frozen pelvis can experience severe leg pain during and around her period. Pain radiating on the course of the sciatic and pudendal nerves is also common. Patients sometimes cannot cross their legs due to deep tissue infiltrated with endometriosis at the pelvic sidewall. Some cannot sit due to tailbone involvement.
Most patients with frozen pelvis complain of severe changes in bowel habits. This could include constipation with episodes of diarrhea, painful bowel movements, and a gassy and bloated feeling.
Patients also report frequent urination (even at night), difficulty holding urine due to decreased bladder capacity, and flank pain caused by an obstructed and dilated ureter.
Most patients at this stage of endometriosis have also stopped having sexual intercourse because of disease involvement in the upper part of the vagina. This causes sex to become incredibly painful during and around the time of a patient’s period. It is also common for pain after sex to continue for several days.
Differences between frozen pelvis and stage 4 endometriosis
Frozen pelvis is different than stage 4 endometriosis and stage 4 adhesions. Most stages of endometriosis are based on a view of the pelvis during surgery with laparoscopy. A pelvic examination by an experienced endometriosis surgeon can easily diagnose frozen pelvis. In other words, while frozen pelvis is a term more commonly used in an initial clinical setting, stage 4 endometriosis can only be formally diagnosed after surgical treatment.
Diagnosis
Pelvic examination in the office is the first step in the diagnosis of frozen pelvis. During the examination, the doctor feels for a firmly fixed uterus. Sometimes the tissues that are frozen in fibrosis involve nerves and blood vessels both in the front and back of the uterus with no mobility at all. As the doctor performs a vaginal examination, a patient with frozen pelvis can feel extreme pain. This is because their pelvic organs have lost all flexibility. This, in turn, causes pain and discomfort due to the nature of the adhesions pulling on other organs.
An endovaginal sonogram must immediately follow the pelvic examination. The aim is to rule out the involvement of the uterus or presence of an endometrioma and confirm the findings of bimanual examination. Due to the fact that pelvic examination is extremely painful, the doctor performs a very gentle evaluation at this stage. A recto-vaginal examination is the last part of the evaluation to check for nodules in the rectum and upper vagina.
After a thorough examination, the next step is to obtain an MRI of the pelvis with contrast to see the depth of involvement and status of the kidney and its outlets, the ureters, and the bladder.
Surgical treatment
Surgery for frozen pelvis is performed using minimally invasive techniques, also known as advanced laparoscopy. All team members must be very experienced surgeons who have mastered their specialty. Each should perform their part in the surgery. The urologist should perform the cystoscopy and stent application into the ureters.
The entire procedure is performed using tiny instruments. These enter small incisions while the image of the surgery is transmitted to a high-definition video screen. This screen is larger than the actual operative field and allows additional zooming-in of the camera. This allows the endometriosis excision surgeon to perform excision with the ultimate precision needed to remove endometriosis scar tissue. A surgeon must flawlessly suture both extracorporeally and intracorporeally with precision and speed.
In addition to experience with the disease, the skill of the lead surgeon and his or her hand and eye coordination, as well as perseverance, has a direct role in ensuring the precise and complete excision of the deep nodules. An expert endometriosis excision surgeon with experience and skill is imperative to treat the extreme condition of frozen pelvis.
Frozen pelvis surgery may last up six hours. It mostly consists of the wide excision of the nodular and infiltrative endometriosis involving the bowel, rectum, and sigmoid colon. Bowel resection, discoid excision, and shaving of lesions with nodulectomy are all possible surgical procedures that may be necessary. The bladder, the ureters on both sides, and the parametrium of the vaginal walls are always affected in frozen pelvis. Therefore, surgery will involve these anatomical locations.
Our approach
Surgery may be performed by laparotomy or minimally invasive surgery, also known as laparoscopic surgery. Rather than a large skin incision over the bikini line or from the belly button to the pubic hair, we prefere the laparoscopic approach where incisions are very small and almost invisible. Altogether only four incisions, most of which only one-fifth of an inch (5 mm) are necessary. If added together, these tiny incisions would total the length of 2.5 centimeters (exactly one inch).
Our surgeons advance from surrounding healthy tissue to contain and encircle the fibrotic tissue. When they locate the ureters safely, they use open anatomic spaces around the bladder and bowels to advance to deeper tissues. Eventually, removal of the disease involves the partial removal of the rectum, bladder, ureter, and significant volumes of nodular fibrotic tissue attached firmly to muscle, fascia, ligaments, arteries, veins, and lastly, nerves. The ultimate principles of microsurgical techniques need to be used due to proximity and involvement of the ureters and nerves, particularly the ischial nerve and parametrial retroperitoneal deep tissues, which are all key for nerve function.
Frozen pelvis is one of the most extreme cases of endometriosis. It is a rare occurrence and the endometriosis scarring is extensive. So, many physicians have trouble treating frozen pelvis due to endometriosis. We have learned that in these cases, it is crucial to listen to all symptoms a patient may present, as these can be key indicators as to where endometriosis scar tissue may lie. As long and intensive as frozen pelvis surgery may be, we stress the importance of removing as much endometriosis scar tissue as possible. Frozen pelvis can cause a great deal of pain in a patient’s day to day life. However, there is no reason that you should be fighting this battle alone.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.
