Endometriosis occurs when tissue resembling the endometrium starts to grow outside the uterus. This usually occurs in or around the reproductive organs. However, in rare cases, the disease can spread to other areas such as the bladder, kidneys, lungs, bowels, and appendix.
It is not clear how common endometriosis of the appendix is, and there is great variation in the rate of appendiceal involvement with numbers ranging from 1 to 22%.
Causes of endometriosis
The exact cause of endometriosis is a mystery. It is also not clear why the disease sometimes spreads to other areas such as the kidneys, diaphragm, or appendix. One hypothesis is retrograde menstruation where the menstrual blood carrying endometrial debris flows backward into the fallopian tubes and subsequently implants and forms lesions.
Other theories include:
- the coelomic metaplasia theory, which suggests that the peritoneal cavity—or the space within the abdomen that contains the intestines, stomach, and liver—houses progenitor cells or cells capable of differentiating into endometrial tissue in response to a specific signal.
- the induction theory, which suggests that the endometrium, or uterine lining which is shed during menstruation, produces substances to form endometriosis.
- the cellular immunity theory, which suggests that alterations in the immune system allow endometrial cells to grow outside the uterus.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Symptoms of endometriosis of the appendix
Appendiceal endometriosis can cause a wide range of symptoms that mimic symptoms of acute appendicitis. These are a sudden pain that begins on the right side of the lower abdomen and that worsens with movement, loss of appetite, nausea, vomiting, abdominal bloating, constipation or diarrhea, and fever. However, unlike acute appendicitis, endometriosis of the appendix usually causes pain that comes and goes with the menstrual cycle.
Patients may also experience:
- symptoms of acute appendicitis
- appendiceal invaginations
- abdominal colic, nausea, and melena, or black stools
- no symptoms
Diagnosis of endometriosis of the appendix
It is difficult to diagnose endometriosis of the appendix because the symptoms are very similar to those of acute appendicitis.
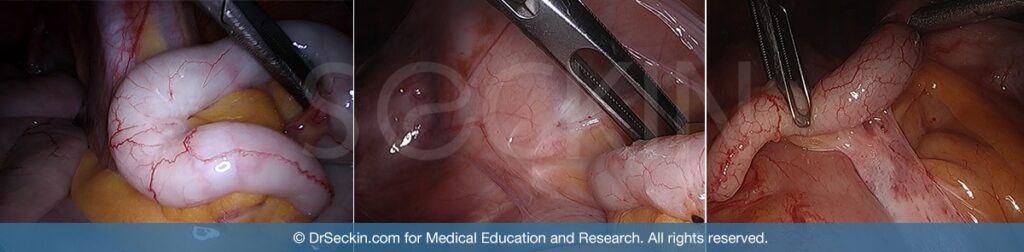
One of the most important tools in diagnosing the condition I a physical examination. However, imaging techniques such as CT scans can also be useful. The surest method for a definitive diagnosis, however, is laparoscopic surgery.
It is very important to diagnose endometriosis of the appendix early so that patients can receive the treatment they need. If left untreated, appendiceal endometriosis can lead to bleeding or perforation in the intestines and obstruction of the bowels.
Treatment of endometriosis of the appendix
An appendectomy (the surgical removal of the appendix) is the best way to treat appendiceal endometriosis. In more severe cases, an ileocecectomy (the surgical removal of the ileum, a part of the small intestine) or hemicolectomy (the removal of a segment of the colon) may be necessary.
The rate of appendiceal involvement of endometriosis varies greatly, ranging from 1% to as high as 22%. Researchers hypothesize that the way in which the specimen is analyzed could partly explain this wide disparity.
Patient story

“Being a freshman in college was enough stress, the last thing I needed was this disease bringing me down. Together, Dr. Seckin, my parents, and I decided surgery was the best option. Going in with no guarantee of success I put all my trust in Dr. Seckin knowing I was in good hands. I am happy to say that now, two weeks after my surgery I feel GREAT! Dr. Seckin removed 15 suspicious adhesions and a very fatty, unhealthy, inflamed appendix. Aside from expected soreness from the surgery, I am confident that I am on the right track back to my old self. ” –Anessa Marinello
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.
