If a woman has fibroids but wishes to preserve her fertility, a myomectomy may be the best procedure. Removing these masses can be a difficult process and requires meticulous planning and attention to detail. At the Seckin Endometriosis Center (SEC), we aim to keep your concerns to a minimum by using different techniques to remove fibroids, including hysteroscopy and laparoscopy.
With over three decades of experience in fibroid procedures, we are confident in the standard techniques that we established for use strictly by laparoscopic surgeons, ensuring almost scarless incisions.
We have also developed our bloodless myomectomy procedure using a unique novel tourniquet technique in addition to standard putrescent for our more complex fibroid operations. This ensures minimal blood loss and stresses the importance of uterine suturing and reconstruction following fibroid removal in order to preserve the uterus and maintain fertility.
While most surgeons offer abdominal myomectomies, which require large incisions, our myomectomy surgery for fibroids guarantees minimal invasion, a short healing time, and nearly scarless results.

What is a myomectomy?
A myomectomy derives from the words myoma (fibroid) and ectomy (to remove). It is a fibroid removal surgery from the uterus. When a woman wishes to preserve the ability to bear children and has fibroids, a myomectomy is usually the best option as it preserves the uterus.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
What are fibroids and where do they grow in the uterus?
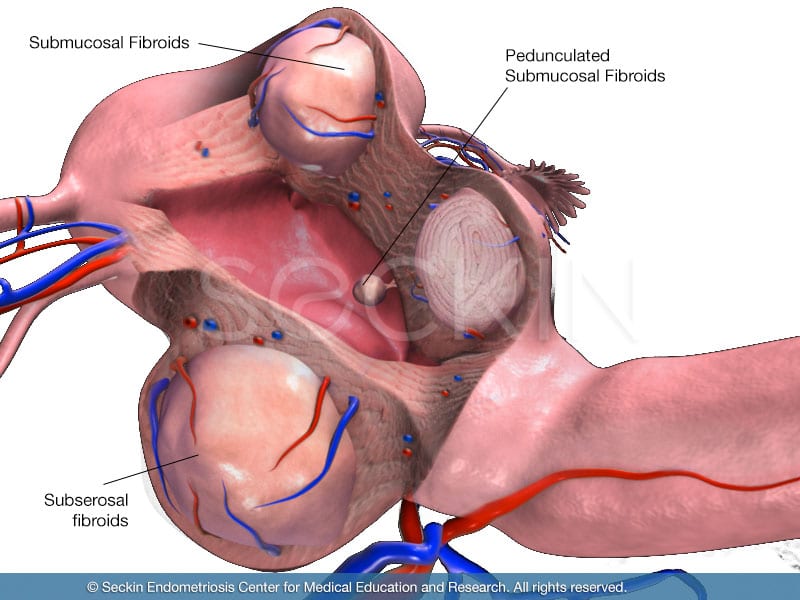
Fibroids are benign fibrous tumors that grow in the muscle layers of the uterus. They can also be called myomas or leiomyoma. It is a common misconception that fibroids are cancerous. They are not. While considered tumors (swollen masses) fibroids are benign (non-cancerous) growths that develop in the uterine muscle. They can grow within the wall of the uterus (myometrium), outside the wall of the uterus, and on a stalk. There are different types of fibroids according to their location.
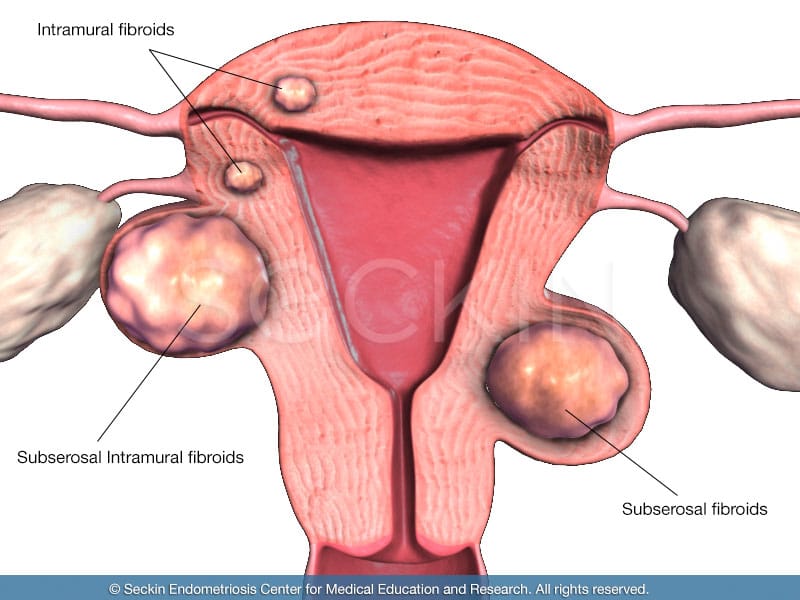
- intramural fibroids located in the thick wall of the uterus (myometrium)
- subserosal fibroids located outside the wall of the uterus
- submucosal fibroids located beneath the lining of the uterus (endometrium)
- intracavity fibroids located within the uterine cavity
- cervical fibroids located in the cervix, the neck of the uterus
- pedunculated fibroids located on a stalk that grows into the uterus or outside the uterine wall
Why is a hysterectomy more common than a myomectomy?
According to US News Health, more than 50,000 myomectomies take place in the U.S. each year. In contrast, surgeons perform 200,000 hysterectomies each year to treat fibroids. About a third of these are to treat fibroids.
A myomectomy is a more invasive procedure than a hysterectomy. While a myomectomy does preserve the uterus and its function, fibroids most often grow within the muscle of the uterus, and excising out the fibroid through a myomectomy procedure requires uterine repair and healing. It also usually requires larger incisions, as the fibroid must be removed through the abdomen.
A hysterectomy, on the other hand, removes the uterus in its entirety and surgeons can perform it more easily through smaller incisions. However, a hysterectomy, while less invasive, should only be performed if the fibroids keep reoccurring and the patient is not looking to preserve her fertility. After a hysterectomy, the patient can no longer bear children.
When to opt for a myomectomy?
The primary reason a myomectomy is performed is to preserve a patient’s fertility. By removing fibroids that are preventing the uterus from carrying a child, a patient is able to preserve their uterus for pregnancy. Submucosal and intramural fibroids are perhaps some of the most common forms of fibroids. Intramural fibroids often make it very difficult for a patient to conceive a child, while submucosal fibroids not only make conception challenging but can also increase a patient’s chances of miscarriage. These fibroids can be removed by myomectomy while preserving the uterus in order to increase a patient’s chances of fertility.
A myomectomy is also more commonly advised in cases of singular fibroids. Whenever a fibroid is removed from the uterine muscle, it requires meticulous uterine repair and healing time. A single fibroid requires less repair and healing time than multiple fibroids.
While most fibroids are located within the muscle of the uterus, there are rare cases where the benign mass is on a stalk (pedunculated fibroid). In these cases, it is much easier to remove the fibroid via myomectomy.
In cases where fertility is no longer an option and fibroids are recurring, a hysterectomy can be an option. Nevertheless, you should always discuss your plans and desires with your doctor in order to ensure that you are both comfortable and fully understand the treatment to come.
Symptoms of fibroids
The following may be symptoms of fibroids:
- heavy and prolonged menstrual bleeding, which can include clots
- the feeling of pressure in the pelvis, which can cause abdominal pain, back pain, and bladder and/or bowel dysfunction
- abdominal bloating
- infertility
- anemia
- fatigue
- dyspareunia (pain during intercourse), which is common in case of cervical fibroids
- deep thigh aches with varicose veins
Around 75% of women who have fibroids report no symptoms. Symptom severity may depend on the size and location of the fibromas.
Diagnostic tests prior to myomectomy

Before a patient can receive a myomectomy, surgeons must make several preoperative evaluations in order to confirm a presumptive diagnosis of fibroids, as well as to ensure the patient is capable of going through a myomectomy procedure.
Laboratory tests
Laboratory tests before a myomectomy are necessary to obtain a patient’s complete blood count (CBC). This is highly important as a myomectomy involves cutting into and then reconstructing and restoring the uterus. While the best surgeons will ensure minimal blood loss, this type of procedure will nevertheless lead to some blood loss in comparison to a hysterectomy. Therefore it is crucial to check a patient’s blood count before conducting a myomectomy
Endovaginal ultrasound
Imaging tests are often highly useful in providing a presumptive diagnosis, especially in the case of fibroids. An endovaginal and abdominal sonogram can help determine the size, number, and location of fibroids within the uterus. This will give your surgeon an understanding of whether a hysteroscopic or laparoscopic myomectomy is necessary.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) produces a much more detailed picture of the body in comparison to an ultrasound. It can distinguish between leiomyomas and other intramural lesions.
Types of myomectomy
There are several different forms of myomectomy procedures, which vary in use based on the size and location of the fibroid. All of the following myomectomy procedures take place in the operating room, under anesthesia.
Hysteroscopic myomectomy
A hysteroscopic myomectomy uses a narrow telescope-like instrument (hysteroscope) that your surgeon inserts into your vagina and passes through your cervix to visualize the uterine cavity. Using just this technique, some experienced surgeons can remove small, superficial fibroids vaginally.
Laparoscopically-assisted myomectomy
This technique is the same as a hysteroscopic myomectomy. However, the surgeon also inserts a laparoscope into your abdomen to ensure the fibroid or the surgery does not extend into the uterine wall. Fibroids that already extend into the uterine wall or are exposed outside the uterine cavity require laparoscopically-assisted myomectomy.
Robotic-assisted laparoscopic myomectomy
While similar in concept to a laparoscopically assisted myomectomy, this procedure uses robotics. However, it is important to note that the skill of your surgeon is the most important thing.
Open abdominal myomectomy
Also referred to as a laparotomy, this procedure makes one large horizontal (“bikini line”) or vertical incision into the abdomen. This gives the surgeon direct access to the uterus. However, it requires the largest incision in comparison to other myomectomy techniques. Therefore, it also involves more scarring and requires a longer time to heal. Some surgeons prefer this technique when fibroids are abnormally large.
Hormone therapy
To lower their patients’ risk of fibroid regeneration and other more harmful diseases following a myomectomy or hysterectomy, doctors often prescribe hormone replacement therapy. These hormone therapies can vary depending on the type of procedure.
Combination therapy for myomectomy
Following a myomectomy, a patient retains her uterus, which surgeons have repaired to preserve its function. In these cases, research has shown that a combination of hormone therapy is key in reducing the risk of uterine cancer. If the uterus is retained and the patient has prescribed just an estrogen-only therapy, they are at grave risk for abnormal growth in the endometrium. However, progesterone in the combination hormone therapy controls the effects of estrogen-induced uterine tissue growth, thus reducing the risk of uterine cancer.
Monotherapy for hysterectomy
If a surgeon removes a patient’s uterus, a low-dose estrogen-only therapy is best. It can help reduce symptoms of menopause while reducing the risk of blood clots or stroke.
Hormone replacement therapy is not for everyone. Surgeons should inform their patients about the risks and benefits of hormone therapy so that they can decide on the right treatment for their particular case.
Risks and complications
Myomectomies have a low rate of complication, especially in the hands of a skilled surgeon. However, like any procedure, there are some risks.
Excessive blood loss
Perhaps the biggest risk of a myomectomy is the potential for blood loss. This is especially relevant in cases of intramural fibroids, where the fibroid is deep within the muscular layer of the uterus. During a myomectomy, the surgeon will need to cut this tissue, which will bleed. It is normal for some bleeding to occur in such procedures, but it also raises the possible risk of excessive bleeding. It is wise to ask your surgeon how they will ensure that this blood loss is minimal.
Pregnancy complications
During pregnancy, the uterus must be able to stretch and expand as the fetus grows. A doctor may recommend a C-section for a patient who has had a myomectomy, due to the risk of rupturing the uterus and undoing the reconstructive work completed after the fibroid operation procedure. This is a highly rare complication, however.
Left-behind scar tissue
Adhesion development is always a cause for concern whenever there is the surgical removal of tissue. These bands of scar tissue can develop in a number of places, from the inside of the uterus to the outside. Scar tissue outside the uterus can block the fallopian tubes and lead to pregnancy complications. Scar tissue within the uterus is much rarer, but it can cause symptoms such as light menstrual periods and difficulties with fertility.
Myomectomy FAQs
How can a myomectomy treat infertility?
A myomectomy is primarily performed to preserve the uterus so it can bear a child during pregnancy. A myomectomy can also increase a woman’s fertility because the fibroids could have been preventing the patient from getting pregnant. This is because fibroids can block the path of a sperm cell through the cervix, uterus, or fallopian tubes. Finally, the type of fibroid could have played a role in the severity of the patient’s infertility. For example, while intramural and cervical fibroids can make it difficult to conceive a child, submucosal fibroids can lead to both complications of conceiving children and miscarriages. A myomectomy is thus a highly useful technique in treating these cases of infertility, as it not only removes the fibroid(s) but also looks to repair and restore uterine function.
What can I expect on the day of my surgery?
Understanding the procedure itself, including the type of myomectomy that you will have, can help you with what to expect the day of surgery. Make sure you understand what you consent to before signing. Asking the right questions will provide the right answers.
Based on your symptoms and preoperative diagnostic tests such as hysteroscopy and sonohysterography, your surgeon should be able to give you a presumptive estimate as to where your fibroid is located, and in turn, the technique that they will use to remove it. While a hysteroscopy and hysteroscopic myomectomy can be part of any myomectomy procedure, the location of your fibroids can lead to different techniques on the day of your surgery. Nevertheless, you must also be aware that this is a presumptive diagnosis and thus every fibroid surgery, whether it is hysteroscopically or laparoscopically performed, may be complicated. This can mean a higher number of fibroids, larger fibroids, and more blood loss than expected. Therefore, it is important to be well informed and ready for your surgery.
Below are a few ways you be as prepared as possible:
Sleep
It is important to get enough sleep the day before your surgery. Being well-rested will not only make you alert prior to your surgery, but it should also make the healing process following surgery much more bearable.
Bowel prep
Have a light meal the night before your surgery. It is common for a surgeon to have their patients conduct bowel preparation, which entails mechanically emptying the bowels the night before surgery as well as not having any food or drink starting at midnight the day of your surgery.
Blood bank
This is very unique to a myomectomy procedure, especially in the case of intramural fibroids. Because your surgeon will cut into and reconstruct the uterus, bleeding will be inevitable, despite your surgeon’s efforts to reduce the amount of blood loss. Therefore it is advised to have a blood bank as a backup in case there is an excessive amount of blood loss in surgery. While this is very rare, it is a highly valid discussion to have with your surgeon in order to gain an understanding of how much blood loss they are expecting in your particular case.
Report daily meds
When you check into the operating room, you will meet the entire surgical team, which includes your surgeon and anesthesiologist, among others. It is important to inform them of the daily medications you may be on, such as beta-blockers, aspirin, coumadin, blood thinners, and antidepressants.
How will each type of myomectomy affect my day of surgery?
| Hysteroscopic myomectomy | Laparoscopically-assisted myomectomy (vaginal route) | Laparoscopically-assisted myomectomy (abdominal route) | Robotic myomectomy | Open myomectomy | |
| Number of incisions | 0 incisions | 2-3 incisions | 4 incisions | 5 incisions (2.5cm) | 1 large incision |
| Size of incisions | No incisions | 1.5-2.5cm (abdominal) incisions | 3 small (1cm) and 1 large (>5cm) incisions | 3 small (7mm) and 2 large (2.5cm) incisions | 5-20cm incisions |
| Length of procedure | <1 hr | 1-3 hrs | 1-3hrs | 2-4 hours | Less than 3 hours (depends on the number of fibroids) |
| Hospital stay | Same day release | 0-1 days | 1-3 days | 1-2 days | 3 days |
| Recovery time | None | Less than a week | 2-4 weeks | 2-4 weeks | 6-8 weeks |
What can I expect the days following my surgery?
The type of myomectomy surgery you undergo will affect your recovery time and any following symptoms. For example, following a hysteroscopic myomectomy, there will be some degree of spotting or a short period.
After laparoscopic myomectomy, on the other hand, there will be some discomfort and pain immediately following surgery, which should resolve over the next few hours. Non-steroid anti-inflammatory drugs (NSAID) and more powerful pain relievers such as Percocet or hydromorphone can help control this pain. However, we do not like to give narcotic oral medication more than one or two days following surgery due to the drug dependency that this medication causes. It can also slow down the GI tract, causing constipation and bladder dysfunction.
Below are other things to be mindful of following your myomectomy surgery.
Diet
We advise light meals, such as soup or juices, for the first day following your surgery. You should stay away from both high protein products like meat and eggs as well as dairies like milk and cheese until you begin passing gas and bowel movements naturally. Once this occurs, you can generally go back to your normal diet.
Movement
Following any surgery, it is crucial to get up and walk as early as possible. Patients who walk as soon as possible, ideally the same day of their surgery, often find they have a much easier time recovering and resuming their normal activities.
Showering
Patients should only shower 24 hours after their surgery. This is to ensure that their incisions have time to heal naturally.
Return
If you experience symptoms like continuously passing gas and painful bowel movements you should return to the hospital. It is highly recommended that you go to the same hospital where you had your surgery as only the team that operated on you will have the best understanding of your case. You do not want other physicians to misdiagnose your case, or worse, rush you into another surgery that could be unnecessary.
Our approach
We have spent over two decades meticulously perfecting our myomectomy technique, which, we cater specifically to your case. Our methods to remove fibroids, depending on their specific classification, include the following.
Intracavitary and submucosal fibroids (hysteroscopic myomectomy)
These fibroids that reside within the uterine cavity and below the surface of the uterine lining, can be removed hysteroscopically. While most surgeons remove these fibroids laparoscopically, we have gained the experience and expertise to perform this technique through the vagina and out of the cervix, which is termed a hysteroscopic myomectomy. By removing these fibroids vaginally, we eliminate the need to make large incisions in the abdomen and ensure that the patient has minimal scarring. We can perform this technique regardless of whether or not the patient has a single fibroid or multiple fibroids.
Intramural and subserosal fibroids (laparoscopic myomectomy)
Unlike intracavity and submucosal fibroids, these masses must be removed with the assistance of laparoscopy. We have great experience in handling large fibroids, having removed fibroids causing the uterus to enlarge to a size equivalent to that of a 22-week pregnancy. Even for laparoscopic myomectomies, we have catered our technique to optimally fit each classification of fibroids.

Pedunculated subserosal fibroids (bead string and culdotomy technique)
When fibroids grow on these stalks, they are easy to remove without causing any harm to the uterus. We conduct this procedure with a loop electrode or single trocar stitch. While it is most common to remove these fibroids through incisions in the abdomen, which surgeons call a “mini-laparotomy,” our preferred method does not require large incisions in the abdomen. By making a small culdotomy incision (vaginal incision), we are able to remove the fibroid vaginally through a natural orifice. We do this by using what we call the beading technique, in which we line fibroids in a bead string, cut them at the base of the stalk, put them in a surgical bag, and then pull the bag out with an instrument shaped like a fish hook. Using this method, we can remove fibroids up to 8-9 cm without any large incisions to the abdomen.
Intramural fibroids (bloodless myomectomy)
Because these fibroids are in the muscular layer of the uterus, they are perhaps the most challenging fibroids to remove. They require a truly specialized myomectomy procedure, which involves a cut on the uterus, as these fibroids can grow to be the size of a football. Our unique method of removing these fibroids is through what we call a “bloodless myomectomy.” Using this procedure, we are able to remove the intramural fibroid while ensuring minimal blood loss and uterine repair and preservation. This technique requires three steps:
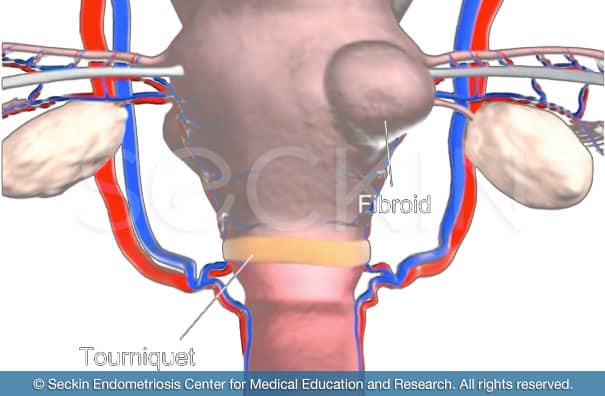
Step 1: “tourniquet technique”
In this step, the blood supply is temporarily cut off from the fibroid, similar to the way a nurse may wrap a rubber band around your arm when they draw blood. This blocks the arterial blood flow to the uterus, ensuring minimal blood spillage during the procedure. Injecting diluted pitressin (8-arginine vasopressin) intramuscularly also prevents uterine bleeding. This combination of the tourniquet technique plus diluted pitressin allows for minimal bleeding as we cut through the muscle of the uterus in order to remove the fibroid buried within.
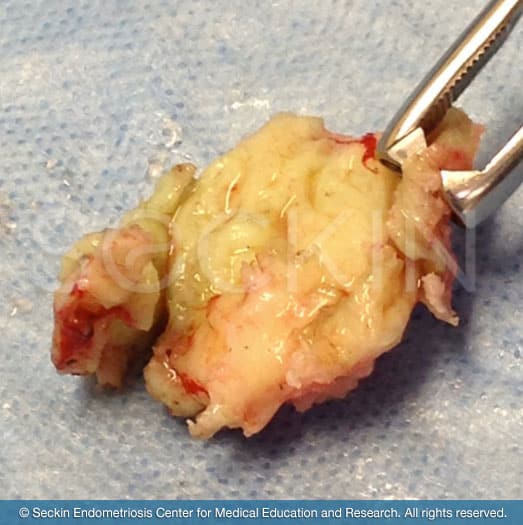
Step 2: enucleation
The second step of a bloodless myomectomy procedure is the enucleation of the fibroid. This is the removal of the fibroid where the mass is neither cut nor dissected. This is to ensure that no smaller pieces are left behind. The fibroid is instead removed in its entirety and then collected in what is called an “endo-bag.”
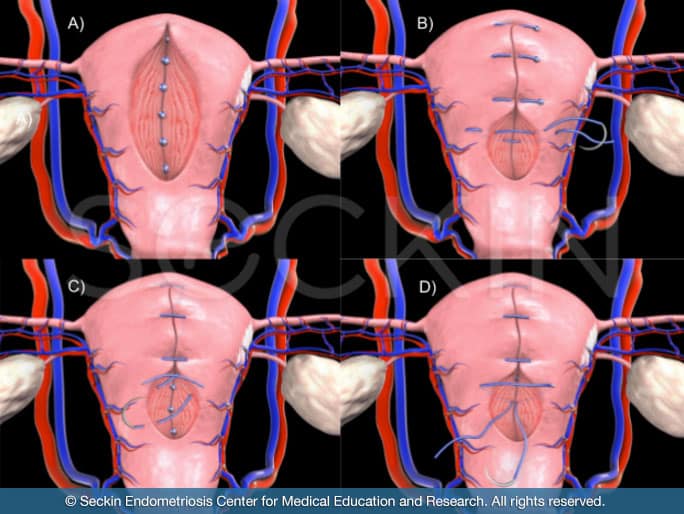
Step 3: uterine repair
Once the fibroid has been removed, it is necessary to suture and reconstruct the uterus in order to preserve uterine function.
Why do we not use morcellation in fibroid removal?
Morcellation is a common technique that surgeons use to remove fibroids. A round knife is used to cut the fibroid piece by piece, which is then removed separately. This method is known to cause blood spillage and other contents, such as leftover fibroid pieces. In fact, recent research studies have shown that when fragments of the myoma are left behind the following morcellation, they can seed and grow (termed parasitic myomas). To avoid this, we have taken great care to master and improve our bloodless myomectomy technique. We also use copious irrigation and an underwater examination following any myomectomy procedure to check for any oozing from the bed of tissue where we removed the fibroid. With these measures, we are able to ensure our patients that blood spillage and leftover fibrous content is not a cause for concern.
Why do we not use robotics in our myomectomy procedures?
While we are trained in the use of robotic surgery, we generally stay away from robotic procedures, especially for myomectomies. One of our major goals in any myomectomy procedure is to limit the amount of blood spillage. With over two decades of experience in removing fibroids, we have ensured that our bloodless myomectomy technique does exactly this. It is a procedure that requires meticulous execution. We, therefore, prefer to have the procedure in our own hands as opposed to operating through robotics. Though robotics can have some benefits, it does not replace the skills of a surgeon who has decades of practice and experience.
A myomectomy is a highly personal surgery, especially in cases where the fibroids are deep within the uterine muscle wall. Therefore, it is crucial to find a surgeon who will treat you with the personalized care and patience that you deserve. Your surgeon should feel comfortable answering any questions you may have, as well as detailing every option you have for treatment. At the Seckin Endometriosis Center, we pride ourselves on keeping our patients informed so they can decide if a myomectomy is the right choice for their particular case.
Patient story
Tracee M was diagnosed with uterine fibroids in 2010. Five years later, she was referred to the Seckin Endometriosis Center, where she underwent a bloodless myomectomy procedure. Read about Tracee’s story here and how her symptoms have since been resolved.
You can read more stories of patients who received myomectomies in our testimonial section.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.