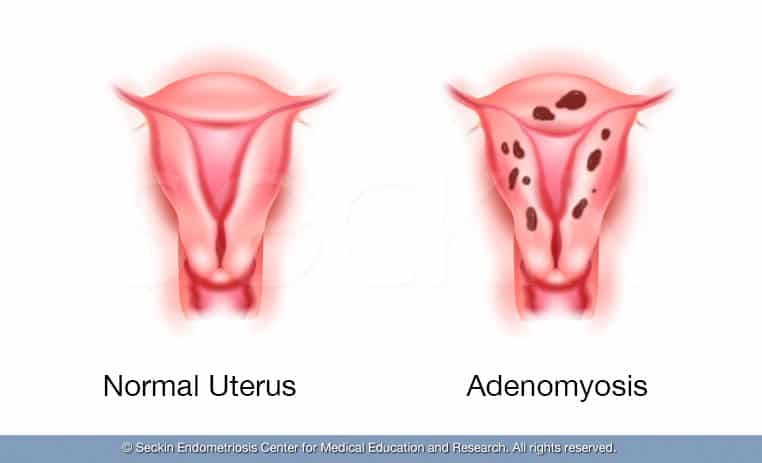
Adenomyosis is a benign disorder of the uterus where the endometrial tissue of the endometrial cavity in the uterus grows into the uterine muscle, damaging the uterine wall. The condition frequently coexists with other gynecological diseases, such as endometriosis and uterine fibroids.
Differences and similarities between adenomyosis and endometriosis
The main difference between adenomyosis and endometriosis is that in endometriosis the tissue grows outside of the uterus.
Both metaplasia conditions, meaning the diseased cells change when they invade new organs. In the case of adenomyosis, this causes abnormal uterine cell growth. Due to these similarities, doctors often refer to adenomyosis as the “sister” disease of endometriosis.
Symptoms of adenomyosis
Like many other diseases, some patients can have adenomyosis, yet have no symptoms at all. Others can experience debilitating pain and heavy bleeding.
Other symptoms of adenomyosis include:
- painful periods and cramps
- heavy menstrual bleeding that includes clots
- painful bowel movements
- bladder symptoms, including uncomfortable urination, burning sensation during urination, or blood in the urine
- peripheral nerve numbness or weakness, which can cause leg or bowel pain during periods
- pain during intercourse
- inflammation of the uterus causing swelling in the abdomen
- deficiency in blood cells or hemoglobin
What causes adenomyosis?
In the last decade, an increasing number of studies have identified various causes for adenomyosis. These include sex hormone receptors, inflammatory molecules, extracellular matrix enzymes, growth factors, and neuroangiogenic factors.
There are many theories surrounding adenomyosis that continue to evolve. Below is a summary of current theories:
- Prior uterine surgery or childbirth causes inflammation of the uterine lining that might cause a break in the healthy boundary of cells lining the uterus. Surgical procedures on the uterus can have a similar effect.
- Tissue trauma or any vaginal injury that allows inflammation can lead to macrophages and cytokines migrating into the myometrium
- High expression of estrogen receptors can stimulate migratory tissue into the myometrium.
- Myometrium cells can spread and build up through the lymphatic system or through stem cells.
- Various hormones including estrogen, progesterone, prolactin, and the follicle-stimulating hormone may trigger the condition.
Factors increasing the risk of adenomyosis
There are several factors that may increase the risk of adenomyosis. These are:
- age with 70 to 80 % of women undergoing hysterectomy for adenomyosis being in their 40s and 50s
- giving birth to two or more babies at the same time or having borne a number of children
- smoking
- ectopic pregnancy
- depression and antidepressant use
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Diagnosing adenomyosis
Pathology
Pathology has always been considered the gold standard to make the final diagnosis of adenomyosis. Generally, women having hysterectomies would have the tissue removed and examined under a microscope by a pathologist.
Imaging techniques
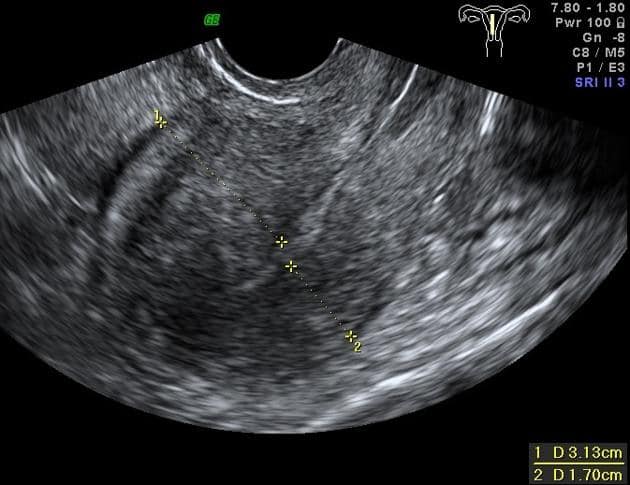
More recently, imaging techniques such as magnetic resonance imaging (MRI) and transvaginal ultrasonography (TVUS ) have emerged as a way for endometriosis specialists to make a non-invasive diagnosis.
An MRI allows a physician to see all the glands of the myometrium, the thickness of the junctional zone (which will be thicker than 1cm in case of adenomyosis), and asymmetric walls. An MRI allows your doctor to see whether or not you have adenomyosis first hand, with a sensitivity rate of 88% and a specificity rate of 93%.
Ultrasound is also highly accurate if performed by an expert sonographer. It can show cysts within the uterine muscle, revealing suspected adenomyosis. An ultrasound can provide substantial enough evidence for an experienced doctor to identify the condition, with a sensitivity rate of 83% and a specificity rate of 85%.
There are also minimally invasive techniques such as historiography, hysteroscopy, cystoscopy, and laparoscopy. However, these are less commonly used for initial diagnosis as they are most often performed in an operating room and are much more expensive.
Classifications of adenomyosis
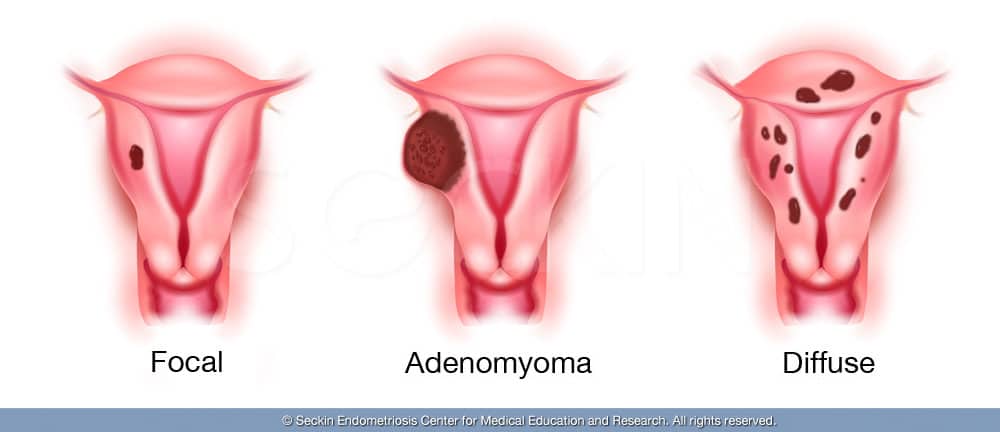
There are three different types of adenomyosis:
- Focal adenomyosis occurs in one particular site of the uterus.
- Adenomyoma is a form of focal adenomyosis, but it is more extensive, as it results in a uterine mass or benign tumor, similar to uterine fibroma.
- Diffuse adenomyosis, unlike the other two types, spreads throughout the uterus.
It is important to correctly identify the type of disease a woman has as the treatment approach will depend on the type of disease. For example, focal adenomyosis and adenomyoma, if operated on correctly, will not require a hysterectomy in most cases.
Does adenomyosis affect pregnancy?
It is common for patients with adenomyosis to have decreased fertility rates and, in some cases, infertility. This is because patients with this disease are more likely to have endometriosis too, which can have detrimental effects when it comes to the reproductive system. When a patient has adenomyosis, the growing myometrium may obstruct the fallopian tubes. A partial blockage of the opening between the uterus and the fallopian tubes will ultimately decrease a woman’s chance of getting pregnant, as this is the path that sperm takes to fertilize the egg.
According to research results presented at the Japan Society of OB/GYN, patients with adenomyosis have a miscarriage rate of 50%, a pre-term birth rate of 24.4%, and a fetal retardation rate of nearly 12%.
Disorders associated with adenomyosis
- About 40 to 50% of patients with adenomyosis also have endometriosis. One in five patients diagnosed with endometriosis after age 30 have adenomyosis or have an increased risk of developing the disease.
- 50% of patients with adenomyosis also have fibroids.
- Patients with adenomyosis often also have anemia, or a deficiency in blood cells or hemoglobin, which results in pallor and a weak appearance.
Treatment of adenomyosis
Surgical treatment
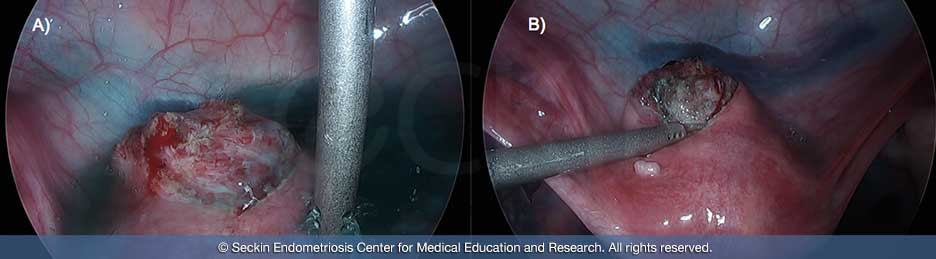
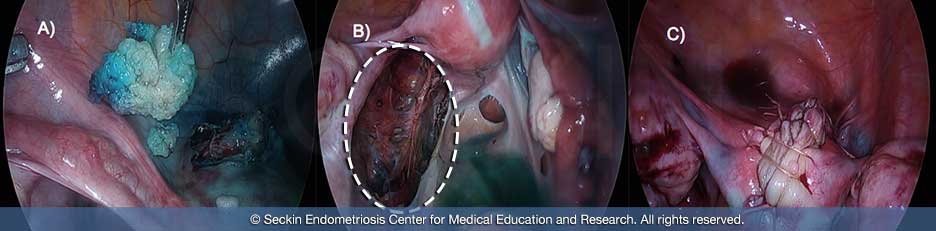
The only way to treat adenomyosis is uterine surgery. The preferred surgical method is laparoscopic deep excisional adenomyosis surgery (LEAS). The aim is to prevent the removal of the uterus. Requiring extreme skill in meticulous suturing, uterine muscles need to be reconstructed layer by layer to allow a future pregnancy.

In cases adenomyosis is confined to one wall, another conservative technique that could be performed is the Osada procedure, named after the Japanese surgeon who developed it.
Alternative surgical methods are hysterectomy or partial hysterectomy. This is when the surgeon removes the whole uterus or part of it. In either approach, any endometriosis, which coexists with adenomyosis in more than half of the cases must be completely excised.
non-surgical treatment
The symptoms of the disease can also be managed non-surgically. The right method for each patient depends on the seriousness of their condition.
Many of the medications approved for and used by endometriosis patients can also be used to treat adenomyosis. However, while some patients experience pain relief by taking birth control pills, others do not. If bleeding is a patient’s primary symptom, birth control pills and/or IUDs may be helpful. The side effects of each medication should be considered, as patients react differently to different medications. Also note that hormonal treatments do not treat adenomyosis, but only manage menstrual cycles.
One method not recommended for treating adenomyosis is uterine artery embolization.
Our approach
Unlike many gynecological surgeons, surgeons at the Seckin Endometriosis Center do not always view hysterectomy as the universal treatment for adenomyosis. In fact, we believe that too many patients undergo unnecessary hysterectomies.
Hysterectomy as a last resort
In cases of focal adenomyosis or adenomyoma, the team will advise a minimally invasive approach avoiding large scar laparoscopic deep excision surgery before a hysterectomy. Only in cases of advanced adenomyosis will Dr. Seckin perform a hysterectomy, because in these cases the abnormal tissue has spread throughout and the uterus is beyond repair.
Removing the uterus with a hysterectomy doesn’t solve all the co-morbidities associated with adenomyosis because nearly 50% of women diagnosed have lesions outside the uterus. A hysterectomy alone addresses neither peritoneal endometriosis nor deeply infiltrating lesions that may associate with the bowel, bladder, ureter, and retroperitoneal fibrosis causing neuropathy.
A hysterectomy also has its limitations when treating adenomyosis that involves peritoneal endometriosis and deep infiltrating lesions related to the bowel, bladder, ureter, and retroperitoneal fibrosis. Patients will also need to have laparoscopic excision surgery to remove the lesions outside of the uterus.
At the Seckin Endometriosis Center, we have a deep respect for the personal journey that comes with deciding to have a hysterectomy. We never recommend this treatment lightly and only see it as the final option after all other courses of action have been exhausted. Because this is such a difficult diagnosis for so many women, we make it our priority to be available to advise and support patients every step of the way.
Patient story
Amy O. was 39 years old when she came to Dr. Seckin. She had heavy periods and severe cramping since age 12 and received a diagnosis of endometriosis and adenomyosis at age 29, after having four different surgeries. After a 27-year battle with her disease, Amy received her final surgery in July 2016. Read more about how Amy feels now.
You can read more patient stories in our testimonial section.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.
